Safety and Efficacy of Hybrid Thoracic Endovascular Aortic Repair for Management of Aberrant Subclavian Artery Complications
Sarah E. Gray, MD, MPH, Salvatore T. Scali, MD, Kristina A. Giles, MD, Dean J. Arnaoutakis, MD, MBA, Martin R. Back, MD, MS, Michol A. Cooper, MD, PhD, Scott A. Berceli, MD, PhD, Gilbert R. Upchurch, MD, Thomas S. Huber, MD, PhD, Javairiah Fatima, MD.
University of Florida, Gainesville, FL, USA.
Objectives:Aberrant subclavian artery(ASA) is a well described aortic arch anomaly and frequently causes dysphagia, Kommerell diverticulum(KD), and/or axial juxta-aortic aneurysmal degeneration. Historically open repair has been performed, which can be associated with significant morbidity. Hybrid surgical approaches utilizing cervical debranching and thoracic endovascular aortic repair(TEVAR) have been described, but there is limited data describing their safety and efficacy. The purpose of this analysis was to describe our experience with management of ASA complications using hybrid TEVAR. Methods:A retrospective, single institution review of a prospectively maintained endovascular aortic registry was performed to identify all patients treated for ASA complications using TEVAR(2002-2018). The primary end-point was technical success(no endoleak/re-intervention/resolution of index pathology). Secondary end-points included complications, endoleak, re-intervention, and survival. Centerline analysis was employed to measure aortic diameters(KD max diameter=opposing aortic outer wall to diverticulum apex). Kaplan-Meier methodology was used to estimate re-intervention and survival. Results:1240 TEVAR procedures were completed for any indication and 18(1.4%)[male-67%; age 59±13 years] with ASA complications as the index pathology were identified. 94%(n=17)had left sided arch+right ASA. All ASAs were in a retro-esophageal position, and 100% had associated KD. Mean preoperative KD diameter was 63±17mm. Elective repair occurred in 89%(n=2, rupture), and all procedures utilized some permutation of cervical debranching+TEVAR with 56%(n=10) being staged. Partial open arch reconstruction was employed in 22%(n=4). No 30-day mortality or spinal cord ischemia complications occurred. A major complication occurred in 22%(4). During follow-up(mean 15±13 months), technical success was 83%, but 44%(8) had evidence of endoleak(Table). 22%(n=4) experienced at least one re-intervention(1-year freedom from re-intervention=75±10%). Median KD diameter decreased by 5mm[IQR -12, 0] with 78%(n=14) experiencing KD diameter stability/reduction in follow-up. Overall survival was 93±6% and 84±10% at one and 3-years, respectively. Conclusions:This experience represents the largest series of hybrid TEVAR revascularization of ASA complications. Although hybrid strategies employing cervical debranching+TEVAR to manage ASA complications appears to be safe and reasonably effective as evidenced by the low perioperative complication risk and positive aortic remodeling, the endoleak rate raises significant concerns about durability. Greater patient numbers and longer follow-up are needed to further establish the role of hybrid TEVAR management of ASA complications. 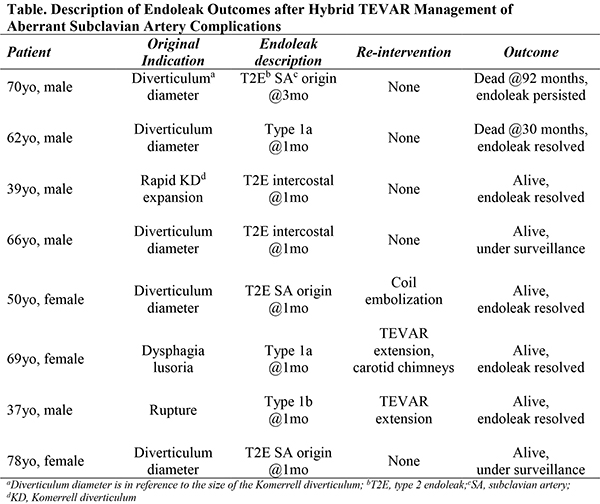
Back to 2019 Abstracts
