Association of Neutrophil-Lymphocyte Ratio with Disease Severity and Outcome after Lower Extremity Procedures
Jonathan Bath, Jamie B. Smith, Robin L. Kruse, Todd R. Vogel.
University of Missouri, Columbia, MO, USA.
Objective: Neutrophil-Lymphocyte Ratio (NLR) has been associated with inferior outcomes after lower extremity (LE) interventions. We examined NLR, severity of peripheral arterial disease (PAD) and outcome following endovascular (ENDO) or open surgical procedures (OPEN). Methods: Inpatients undergoing ENDO or OPEN procedures (2008 to 2016) were selected from Cerner HealthFacts® database using ICD-9 procedure codes and grouped into claudication (Claud), rest pain (Rest) and tissue loss (TLoss). Outcomes were identified using ICD-9 codes with NLR calculated pre-and postoperatively. Chi-square analysis and logistic regression were performed and ROC analysis determined the cutoff for preoperative (Low <3.65; High >/= 3.65) and postoperative (Low <5.96; High >/= 5.96) NLR values. Results: 3530 patients were evaluated; 2028 (57%) underwent ENDO and 1502 (43%) underwent OPEN. Claud was more frequent in white patients (81.7% vs. 72.7%; p<0.0001) and TLoss in black patients (20.9% vs. 12.9%; p<0.0001). Increasing severity of PAD led to longer hospital stay (Claud 2.3d vs. Rest 4.1d vs. TLoss 6.4d; p<0.0001). Preoperative High NLR was seen in 36.6% of patients; more commonly in older patients (70 vs. 67; p<0.0001) and with higher Charlson Index (3.2 vs. 2.5; p<0.0001). Mean pre- and postoperative NLR increased significantly with PAD severity (Figure 1.) Mean pre- and postoperative NLR was higher for OPEN than ENDO across Claud, Rest and TLoss. Logistic regression revealed preoperative high NLR was strongly associated with in-hospital death (OR 5.4, 95% CI 1.68-17.07), renal failure (OR 1.9, 95% CI 1.18-2.93), cardiac complications (OR 2.9, 95% CI 1.57-5.40), respiratory complications (OR 1.7, 95% CI 1.09-2.76), amputation (OR 2.5, 95% CI 1.65-3.87) and prolonged length of stay (OR 1.9, 95% CI 1.89-3.71). Conclusions: Pre- and postoperative NLR significantly increases with disease severity for PAD. After adjusting for confounders, NLR still remained strongly predictive of death, cardiac events, respiratory failure, renal failure, amputation and increased length of stay for patients undergoing LE procedures. NLR is an inexpensive biomarker that predicts inferior outcome and could be used to assist providers with clinical decision making and risk stratification when considering LE procedures. 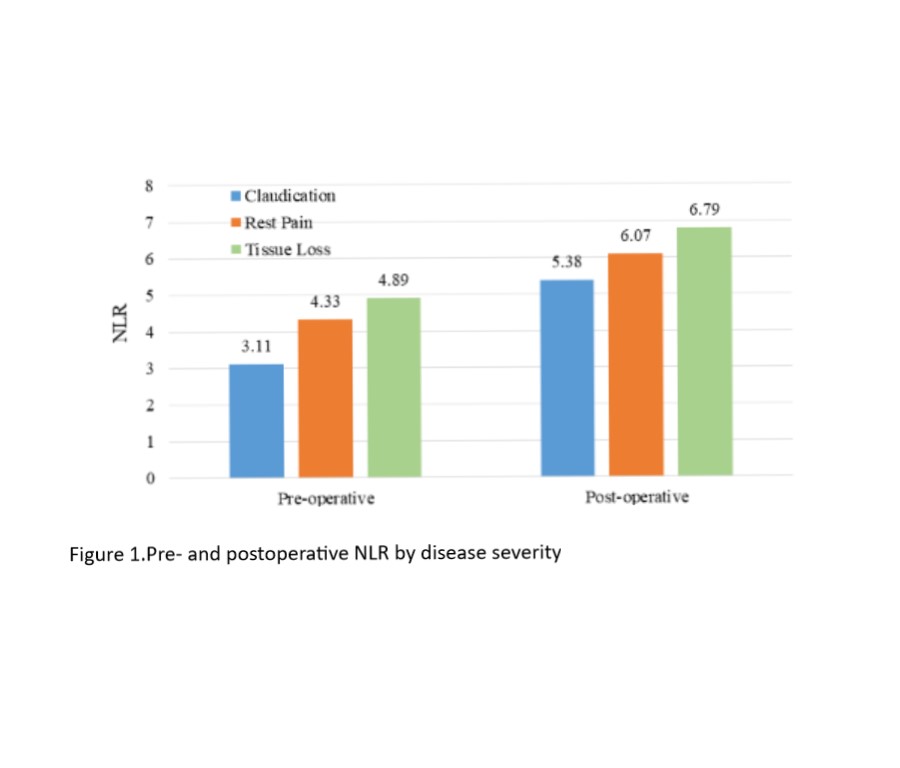
Back to 2019 Abstracts
