Medicare Reimbursement for Common Vascular Services: Practice Patterns and Interstate Variation
William W. Sheaffer, MD, Samuel R. Money, MD, William M. Stone, MD, Victor J. Davila, MD, Andrew J. Meltzer, MD.
Mayo Clinic in Arizona, Phoenix, AZ, USA.
OBJECTIVES: The shift from traditional open vascular surgery to endovascular interventions has dramatically altered the practice of vascular surgery. The purpose of this study was to explore the implications of the “endovascular revolution” on the vascular surgery workforce and characterize contemporary practice patterns and reimbursement for common vascular procedures across the United States. METHODS: Vascular surgeons in the United States were identified in the 2016 Medicare Physician Clinical Utilization Data file. All charges and payments to vascular surgeons for commonly performed (>10/year) services were stratified into 10 distinct categories. Charges and payments for these commonly performed services were calculated at the provider, category, and state level. Statistical analysis including ANOVA, Control Chart analysis, and Fisher’s Exact Test were utilized to compare payments and charge:payment ratios. RESULTS: In 2016, vascular surgeons received $592M for commonly performed vascular services. Amongst all categories, endovascular procedures accounted for the greatest proportion of all payments ($226M, 38%) in comparison to open vascular procedures accounting for only 4% ($21M). Vascular lab services ($125M, 21%), varicose vein treatments ($56M, 9%), and access procedures ($49M, 8%) were also of significant contribution (Figure 1). Per category, varicose vein treatments had the highest payment per treatment ($993), followed by open ($753), and endovascular ($638). Evaluation and management charges accounted for 17% ($102.4M) of payments. At the state level there was significant variation in total vascular surgery payments, median vascular surgery payments, and payments per service. The 30 surgeons comprising the top 1% of Medicare reimbursement accounted for 15% ($86M) of medicare payments to vascular surgeons in 2016. CONCLUSIONS:
Open vascular procedures now account for a small fraction of medicare payments to vascular surgeons in comparison to endovascular services and payments for noninvasive studies. While total vascular surgery payments at the state level are expected to be population dependent, there remains significant variation in median payments per surgeon as well as average payment per service in interstate analysis. This study of modern vascular practice highlights the financial impact of the endovascular revolution, the significant variation in reimbursement by location and practice patterns, and the dramatic overlap in services provided by competing specialties. 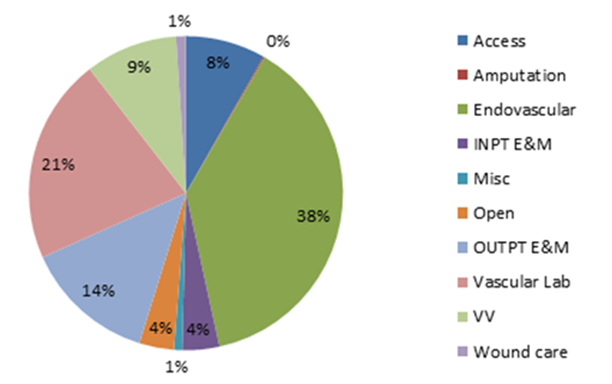
Back to 2019 Abstracts
