Beware the Negative Stress Test: Postoperative Cardiac Events May Be More Prevalent Than in Patients Without a Preoperative Workup
Jesse A. Columbo, MD, MS1, Ravinder Kang, MD, MS1, Douglas W. Jones, MD2, Bjoern D. Suckow, MD, MS1, Daniel B. Walsh, MD1, Richard J. Powell, MD1, Salvatore T. Scali, MD3, Philip P. Goodney, MD, MS1, David H. Stone, MD, MS1.
1Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA, 2Boston Medical Center, Boston, MA, USA, 3University of Florida Health, Gainesville, FL, USA.
Objectives: Patients thought to be at elevated perioperative risk are often selected to undergo stress testing prior to vascular surgery. The objective of this study was to compare the incidence of postoperative cardiac events among patients with negative stress tests versus those who did not undergo testing.
Methods: We reviewed all patients who underwent elective open abdominal aortic aneurysm repair (OPEN), suprainguinal bypass (SUPRA), endovascular aneurysm repair (EVR), carotid endarterectomy (CEA), and infrainguinal bypass (INFRA) within the Vascular Study Group of New England (VSGNE) from 2003-2017. Next, we excluded patients with positive stress tests(n=3,312) and studied two mutually exclusive groups: elective surgery patients with a negative stress test, and elective surgery with no stress test (total n=27,270) The primary outcome was a composite of in-hospital postoperative cardiac events (dysrhythmia, heart attack, heart failure) or death.
Results: A preoperative stress test was obtained in 66.3% of OPEN, 42.8% of SUPRA, 37.1% of EVR, 36.0% of CEA, and 31.2% of INFRA. The crude odds ratio (OR) of in-hospital postoperative cardiac event or death was 1.37(95% confidence interval (CI): 1.07-1.76) for OPEN, and 1.52 (CI: 1.13-2.03) for SUPRA, indicating that patients with negative stress tests prior to these procedures were 37% and 52% more likely to suffer a postoperative event or die compared to patients selected to proceed directly to surgery without testing (Figure). Conversely, the crude OR was 0.92 (CI: 0.66-1.29) for EVR, 0.92 (CI 0.70-1.21) for CEA, and 1.13 (0.90-1.40) for INFRA, indicating that patients undergoing these procedures had a similar likelihood of an event, whether they had a negative stress test or proceeded directly to surgery without a stress test. Adjustment for age, sex, and comorbidities did not meaningfully change these estimates.
Conclusions: Patients are often appropriately selected to proceed directly to surgery within the VSGNE. However, a negative preoperative stress test must not assuage the concern for an adverse outcome, as these patients retain a substantial likelihood of cardiac events, especially after large magnitude procedures. 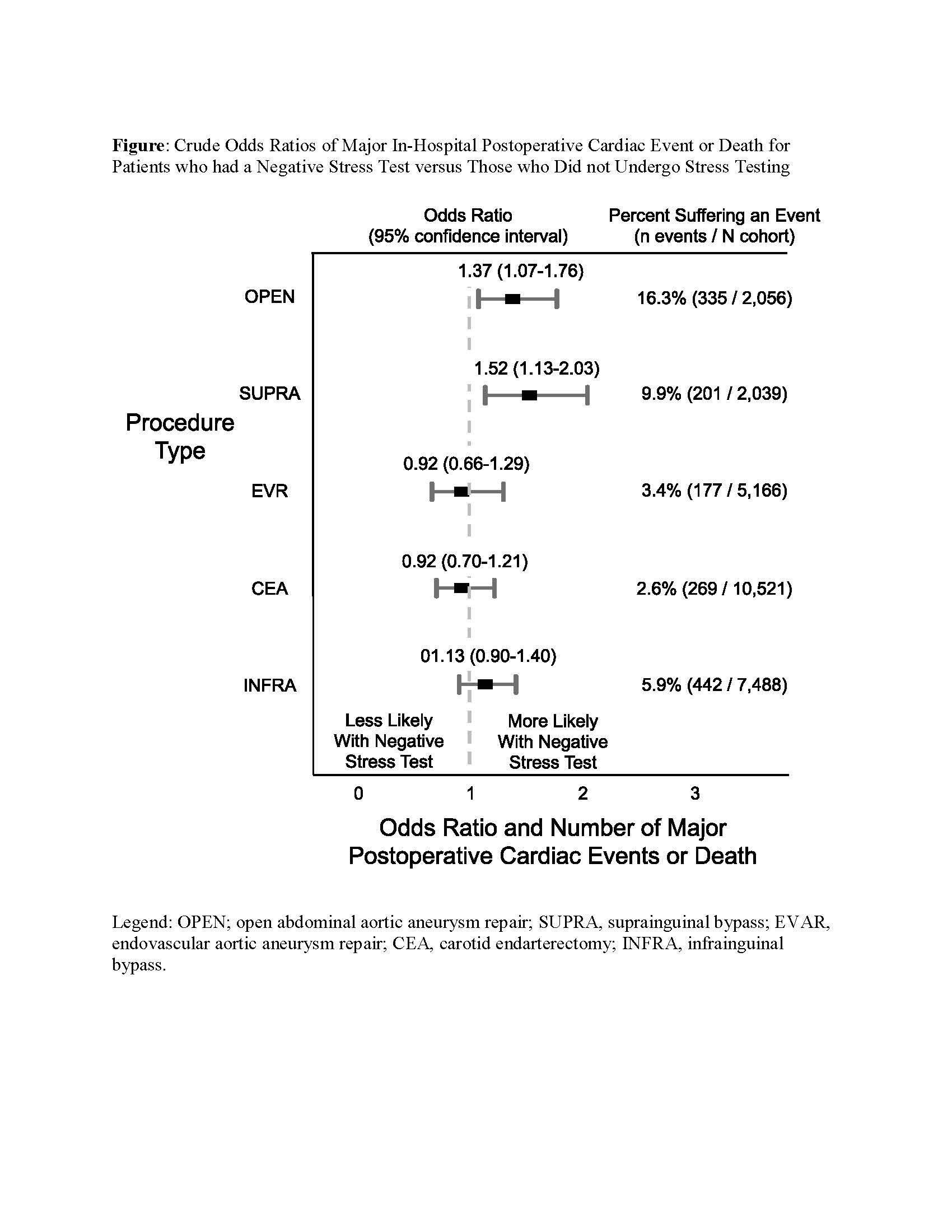
Back to 2019 Abstracts
