Influence of Race In Patterns of Presentation and Outcomes in Patients With Uncomplicated Type B Aortic Dissection
Matthew Aizpuru, BA, Xiaoying Lou, MD, Jaime Benarroch-Gampel, MD, Zachary J. Grady, BS, William D. Jordan, Jr., MD, Bradley G. Leshnower, MD, Robert S. Crawford, MD.
Emory University, Atlanta, GA, USA.
OBJECTIVE:
The relationship between race and outcomes in uncomplicated type B aortic dissection (uTBAD) is not well understood. Recent studies suggest worse long-term outcomes for White patients (Wh) with uTBAD compared to African American patients (AA). Using a tertiary referral center dataset, we sought to determine racial differences in patterns of presentation and outcomes for patients with uTBAD.
METHODS:
Between 2000 and 2016, 353 patients (227 AA, 126 Wh) presented with TBAD at our institution. Of these, 276 (178 AA, 98 Wh) had uncomplicated TBAD. Data were collected on risk factors, major post-operative complications (stroke, renal failure, spinal cord injury) and long-term all-cause mortality. Univariate and Kaplan-Meier survival analyses were performed to identify differences between AA and Wh patients with uTBAD.
RESULTS:
There were no racial differences in the distribution of uncomplicated versus complicated dissection [n=178,(78.4%) vs. n=98,(77.8%);p=0.89]. All uTBAD patients received optimal medical management as first-line treatment. At time of presentation, AA with uTBAD were younger [55.6±11.2 years vs. 59.3±12.7 years;p=0.02], had higher rates of diabetes [n=38,(21.3%) vs. n=6,(6.1%);p<0.01] and end stage renal disease [n=27,(15.2%) vs. n=2,(2.0%); p<0.01]. Wh were more likely to have a history of myocardial infarction [n=8, (8.1%) vs. n=5, (2.8%); p=0.05]. AA had lower rates of intervention [n=70,(39.3%) vs. n=55,(56.1%);p<0.01]. Kaplan-Meier analysis demonstrated Wh were more likely to have failed medical management (death or intervention) by 5 years [51% vs 68%;p=0.05]. The indications for intervention were aneurysmal size [n=60,(86%) vs. n=45,(83%)], pain [n=5,(7%) vs. n=7,(13%)], malperfusion [n=3,(4%) vs. n=2,(4%)] and rupture [n=2,(3%) vs. n=0], and were not different across races (p=0.45). Of those who received intervention, AA underwent more open operations [n=35,(50.0%) vs. n=18,(32.7%),p=0.05] and had a higher rate of pooled major post-operative complications or death [n=18,(25.7%) vs. n=4,(7.2%);p<0.01]. There was no significant difference in survival between AA and Wh patients at 5 [76% vs 71%;p=0.21] or 10 years [54% vs 45%;p=0.17].
CONCLUSIONS:
Although AA presented younger and with increased co-morbidities, Wh patients more often failed medical management over the long-term. Further research is needed to better understand why these differences exist and how they might influence treatment strategies. 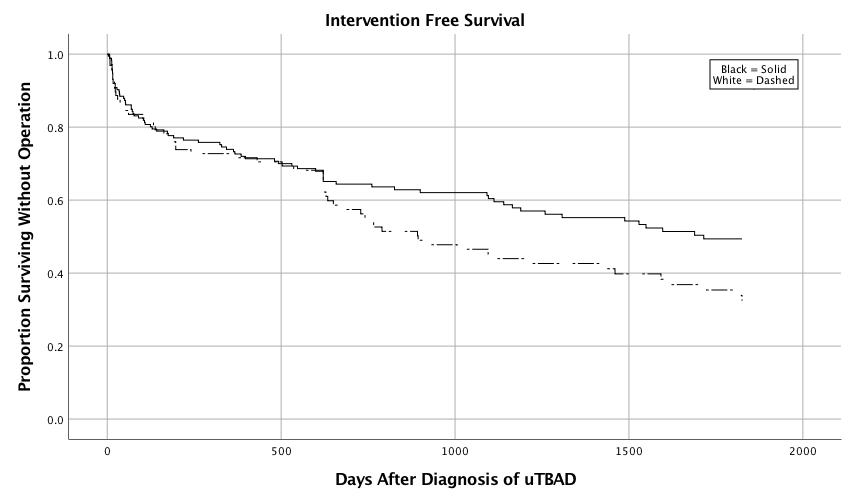
Back to 2019 Abstracts
