The Impact of Frailty Syndrome Measured by 5-Factor Frailty Index in Carotid Endarterectomy
Bradley Trinidad, MD.
Banner University-University of Arizona, Tucson, AZ, USA.
OBJECTIVES: Frailty is highly prevalent in the geriatric population and confers high risk for morbidity and mortality after operative intervention. The aim of the this study was to assess the impact of frailty on outcomes after carotid endarterectomy (CEA) in geriatric patients utilizing the 5-Factor modified frailty index.
METHODS: An 8-year (2005-12) analysis of NSQIP. Patients undergoing CEA for carotid artery stenosis were analyzed. Patients who were 65 years or older were included in the study. The newly developed 5-factor modified frailty index (mFI) was utilized to measure frailty status among patients. The 5-factor modified frailty index items include; Chronic obstructive pulmonary disease; Congestive heart failure; Hypertension; Diabetes; and Partial/total dependence. Patients were stratified into 3 groups based on their mFI: 0, 1, or ≥2. Outcome measures were complications, mortality, failure to rescue (FTR), and hospital length of stay.
RESULTS: 36,090 patients were included in the analysis. Mean age was 74.6±5.9 years. 20.7% of the patients had a mFI ≥2. 10.7% of patients had complications, 3.1% died, and 6.2% were readmitted after discharge. Patients with mFI ≥2 had higher complication rates (21.5% vs. 11.3% vs. 6.2%, p<0.001), higher mortality (5.9% vs 2.1% vs. 1.0%, p=0.02), higher FTR (12.1% vs 5.4% vs. 4.7%, p=0.02) compared to patients with mFI of 1 and 0, respectively. Patients with mFI ≥2 had a longer hospital length of stay (3 [2-3] vs. 2 [2-3] vs. 1 [1-2] days, p=0.02) and a higher 30-day readmission rate (14.5% vs. 10.2% vs. 3.6%, p=0.03) compared to patients with mFI of 1 and 0, respectively. On regression analysis after controlling for age, gender, albumin level, type of surgery, and ASA class, mFI ≥2 was an independent predictor of complications, mortality, and FTR, and 30-d readmissions (Table 1).
CONCLUSIONS:
Geriatric patients undergoing carotid endarterectomy (CEA) with mFI ≥ 2 have higher rates of complications and mortality. The newly developed 5-Factor modified frailty index instead of age alone should be used to guide risk stratification, perioperative optimization, and counseling and while considering treatment options for patients with carotid artery stenosis. 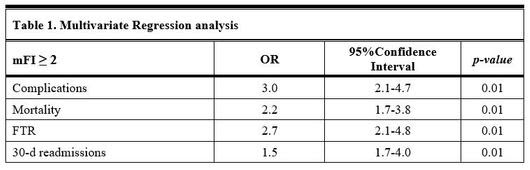
Back to 2019 Abstracts
