Identification of Factors Driving Increased Length Stay after Elective Carotid Endarterectomy
William P. Shutze, Sr., MD1, Anupama Vasudevan, BDS, MPH, PhD2, Roshe Nodine, BAAS1, Rachel Rendon, BA3, Salvatore T. Scali, MD4.
1The Heart Hospital Baylor Plano, Plano, TX, USA, 2Baylor Heart and Vascular Institute, Dallas, TX, USA, 3Texas Vascular Associates, Plano, TX, USA, 4University of Florida, Gainesville, FL, USA.
Introduction: The aim of this study was to investigate the risk factors for delayed (>1 day) discharge after carotid endarterectomy (CEA).
Methods: All patients who underwent elective, CEA in the Vascular Quality Initiative (VQI; 2012-2017) were reviewed. We excluded patients with Non-US insurance, emergent/urgent procedures, ASA class 5, concomitant CABG, proximal/distal endovascular procedures, CEA as part of other arterial operation, prior ipsilateral CEA, death during admission, missing information, centers with number of subjects <30, subjects with a preop LOS >30 or postop LOS >300 days. The primary outcome was discharge after POD 1. Secondary outcomes included in-hospital major adverse cardiac events (MACE), defined as the occurrence of myocardial infarction, stroke, (but not death). Multivariable logistic regression was used to identify predictors of increased LOS>1 day. Two models were constructed to account for preoperative, as well as intraoperative/postoperative risk factors influencing the outcome.
Results: 72,846 patients were analyzed. Group 1 consisted of 52,093 (72%) patients who were discharged by POD1 while Group 2 (discharged ≥ POD 2), contained 20,753 (28%) subjects. There were no significant differences between cohorts for prior history of contralateral CEA, carotid stent, aneurysm repair, neck irradiation, or VQI region/center distribution. Significant differences were evident between the two groups for several other factors (significant to p<0.001) highlighted in Figure 1. Multivariable model 1, identified multiple preoperative risk factors independently associated with delayed discharge as depicted in Figure 1. The strongest preoperative predictors for delayed discharge were female gender, CHF, dialysis-dependence, nursing home living status, need for assisted ambulation, prior remote history of neurologic event and preoperative LOS. Multivariate model 2, accounting for pre-/intra- and postoperative variables verified Model 1ís risk factors and identified MACE as the strongest predictor for delayed discharge followed by postoperative hyper/hypotension. Local and regional anesthesia were associated with early discharge.
Conclusions: In the VQI almost 30% of patients are discharged after POD 1 following elective CEA. Several preoperative patient related and perioperative physiological risk factors are identified that can be used to target efforts to improve patient selection, as well as to invest resources into streamlining processes of care to reduce overall CEA LOS. 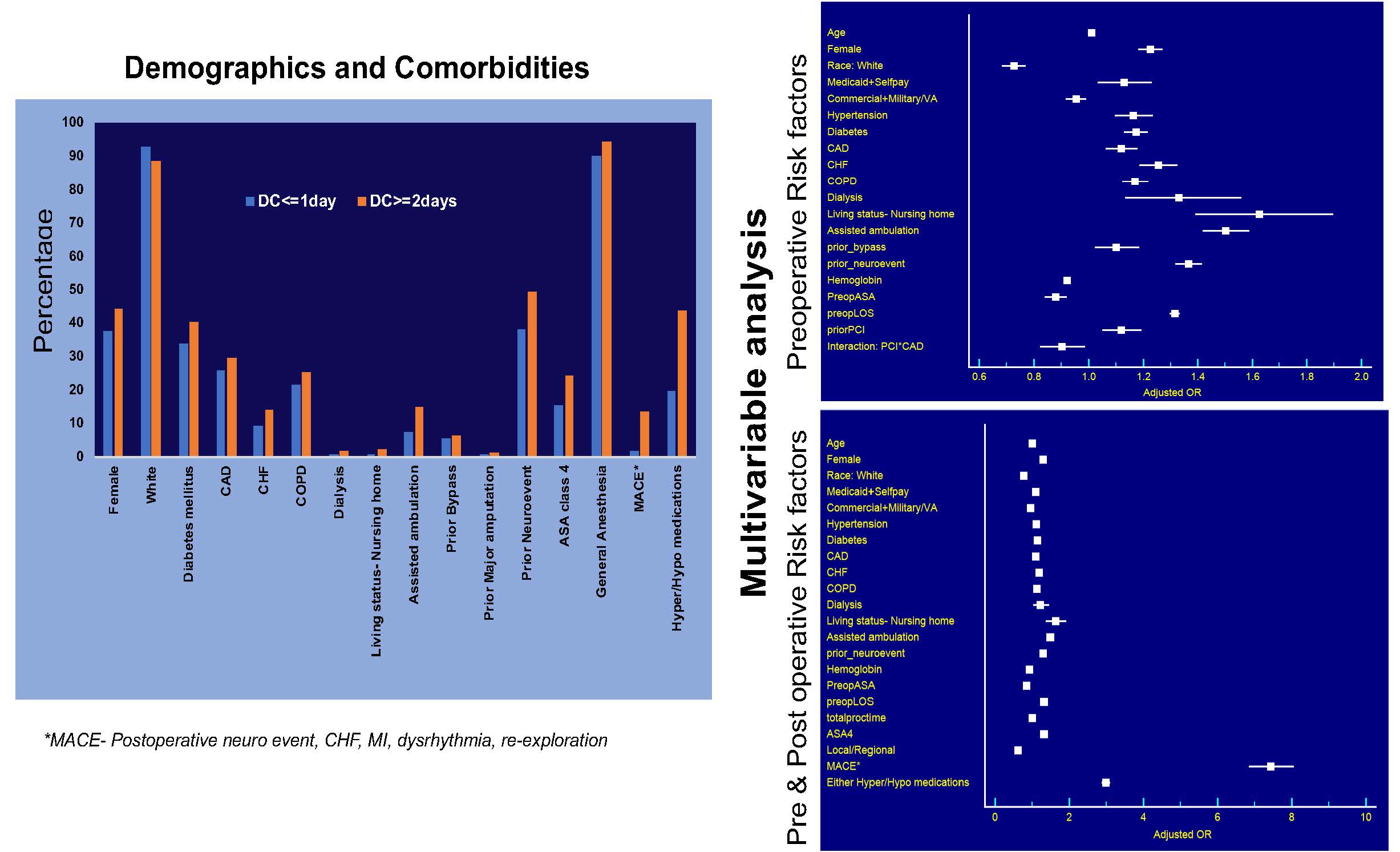
Back to 2019 Abstracts
