Carotid Artery Disease in Hispanics
Rachel Rendon, BA1, Aaron Y. Kluger, MPH2, Kristen M. Tecson, Ph.D2, Anupama Vasudevan, BDS MPH Ph.D2, John F. Eidt, MD3, William P. Shutze, Sr., MD4.
1Texas Vascular Associates, Plano, TX, USA, 2Baylor Heart and Vascular Institute, Dallas, TX, USA, 3Texas Vascular Associates, Dallas, TX, USA, 4The Heart Hospital Baylor Plano, Plano, TX, USA.
Introduction: We aimed to assess the trends in carotid artery disease (CAD) diagnosis and carotid endarterectomy/carotid artery stenting (CEA/CAS) utilization in Hispanic individuals compared to the 2 primary racial groups in north Texas, an area experiencing rapid increases in the Hispanic population.
Methods: We obtained racial/ethnic demographics for the Dallas-Fort Worth (DFW) metroplex and performed a retrospective analysis on the DFW Hospital Councilís clinical data, which incorporates information from approximately 30 hospitals in DFW. The study timeframe was 2006-2017 and inclusion criteria consisted of age >50 years and White, Black, or Hispanic race/ethnicity. Baseline demographics (age, sex, race/ethnicity) and clinical factors (tobacco use, diabetes mellitus, hyperlipidemia, hypertension, cerebrovascular disease, prior stroke), as well as CEA/CAS were abstracted. Differences were assessed via Kruskal-Wallis or Chi-Square tests; trends over time were assessed via Cochran-Armitage tests.
Results: There were 93,518 patients with CAD identified (White 73.4%, Black 17.5%, Hispanic 9.2% ). There were significant group differences in all demographic and clinical factors (Figure 1). The rates of CAD diagnosis were 0.49%, 0.59%, and 0.28% and the procedural rates for those with CAD were 10.3%, 2.8%, and 5.5% for Whites, Blacks, and Hispanics (pís <0.0001). The rate of Hispanic individuals in the DFW metroplex increased from 14.2% to 17.9% over time (p-for-trend <0.0001), but a corresponding increase in the proportion of Hispanics comprising the CAD population was not observed (7.5% to 8.9%, p-for-trend = 0.7358). Despite the increased proportion of Hispanics in the metroplex, the proportion of Hispanics comprising the CEA/CAS-treated population did not change (4.9% to 5.9%, p-for-trend = 0.3087) (Figure 1). All patients were more likely to receive CEA than CAS. A significant relation was detected between race and procedure type (CEA rates: 80.3%, 72.1%, and 74.6% for Whites, Blacks, and Hispanics, respectively; p <0.0001). Additionally, the proportion of CAS cases increased from 15.5% to 22.4% over time (p-for-trend <0.0001).
Conclusions: Hispanics represent an increasing portion of the population in DFW, but there has not been a comparable increase in the percentage of Hispanic ethnicity among those diagnosed with or treated for CAD suggesting that Hispanic individuals may be undertreated for CAD. 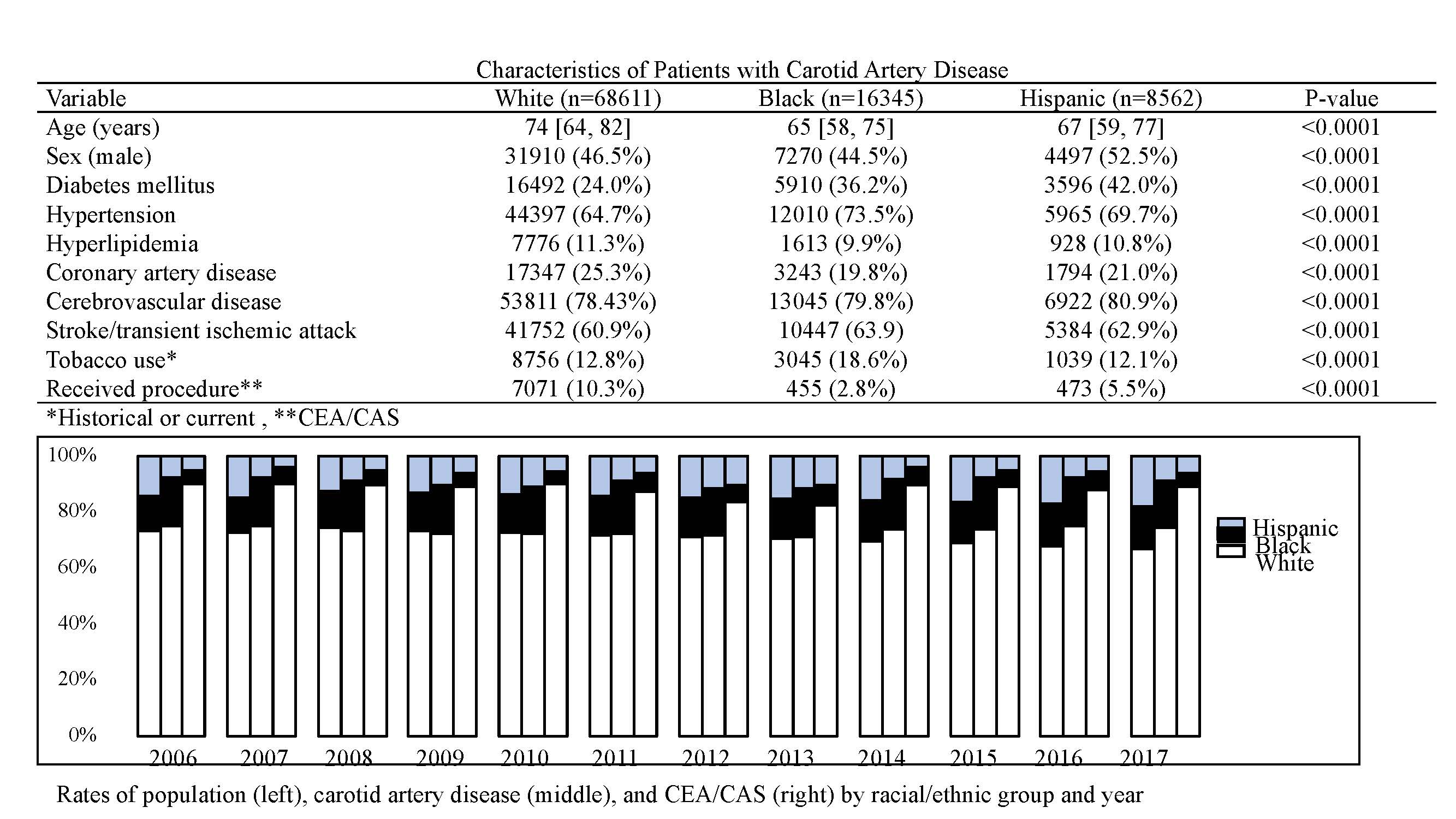
Back to 2019 Abstracts
