Evolution of the Integrated Vascular Surgery Curriculum
Alykhan Lalani, MD, Malachi G. Sheahan, MD, Donald Mendoza, MD, Nicolas Zea, MD, Marie Unruh, MD, Amit Chawla, MD, Amadis Brooke, MD, Claudie Sheahan, MD.
Louisiana State University Health Sciences Center, New Orleans, LA, USA.
OBJECTIVES: Integrated residencies in vascular surgery began in the United States in 2007. Other than a minimum 18-month requirement for “core” surgery, there are few restrictions on the trainees’ rotations. Our goal was to quantify and classify the training experiences of U.S. Integrated Vascular Surgery Residencies.
METHODS: Of the programs participating in the 2019 match, complete rotation schedules and a follow-up survey were obtained from 50 of 54 (93%). Rotations were classified as vascular surgery (VS), core surgery (CS), or non-operative/critical care rotations (NO). CS included general surgery and surgical sub-specialties. NO included vascular lab, ICU, and other non-surgical specialties.
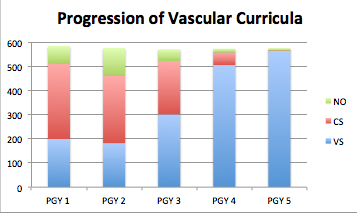
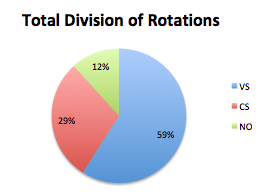
RESULTS: The overall breakdown of rotation schedules was VS 60.8% (1751/2879 months), CS 30.1% (866/2879), and NO 9.1% (262/2879). The most common NO rotations were vascular lab 38% (19/50 programs), interventional radiology 20% (10/50), and cardiology 16% (8/50). Rotation schedule by post-graduate year is shown in figure 1. Total residency time broken down by rotation type is demonstrated in figure 2. In a follow-up survey, with regard to curriculum changes made to the original Program Information Form, cardiology was cited as the most frequently removed rotation and vascular lab was the most frequently added. Critical care and vascular lab were seen as the most important NO rotations and trauma surgery as the most important CS rotation. The most common barrier preventing program directors from expanding their resident complement was lack of funding. Even though integrated vascular trainees are eligible to spend 42 months of their residency in vascular surgery rotations, current schedules provide an average of only 30.17 (Range 25 - 44) months, including vascular lab. CONCLUSIONS: Review of current curricula reveals that integrated vascular residents spend a significant amount of time on non-vascular and non-operative rotations. In light of the declining numbers of open vascular procedures, further studies are required to evaluate these practices and balance the appeal of offering a broad-based curriculum with the reality of training technical competent vascular surgeons.
Back to 2019 Abstracts
