TEVAR Improves Survival Despite Otherwise Dismal Outcomes in Complicated Type- B Aortic Dissection
James C. Iannuzzi, MD, MPH1, Sahael M. Stapleton, MD2, David Chang, PhD2, Yanik J. Bababekov, MD2, Laura T. Boitano, MD2, Richard M. Green, MD3, Hiroo akayama, MD, PhD3, Virendra I. Patel, MD, MPH3.
1University of California San Francisco, San Francisco, CA, USA, 2Massachusetts General Hospital, Boston, MA, USA, 3Division of Cardiac, Thoracic, and Vascular Surgery, NewYork-Presbyterian / Columbia University Irving Medical Center / Columbia University Vagelos College of Physicians & Surgeons, New York, NY, USA.
Obective:
Complicated type-B aortic dissection (CTBAD) is a rarely studied yet highly lethal condition. How mortality and survival has changed with the introduction of thoracic endovascular aortic repair (TEVAR) is unknown, therefore, we evaluated CTBAD outcomes after medical therapy alone (MED) open surgical repair (OPEN), and TEVAR.
Methods:
The California Office of Statewide Hospital Planning Development database (2000-2010) was queried for cases of acute type-B aortic dissections, which were designated CTBAD if they presented with bowel ischemia, lower extremity ischemia, acidosis, shock, or acute renal failure. Bivariate, multivariable, and survival analyses were performed as appropriate to the data.
Results:
Of 1945 CTBAD cases, 91% were treated with MED, 5.2% Open, and 4.0% with TEVAR. Cinical presentation included 31% acidosis, 15% shock, 73% acute renal failure, and 9% bowel or lower extremity ischemia. Mean age was 66±15 years, females represented 36%, underrepresented minorities 33%, and 28% had Charlson score>3. Overall inpatient complication rate was 83%, paraplegia occurred in 3.3%, respiratory complications in 29%, hemorrhage in 8%, sepsis in 12%, acute renal failure in 73%, bowel ischemia in 5.7%, and lower extremity ischemia in 1%. Length of stay was 13±19 days for MED and 24±24 days OPEN, and 21±18 days TEVAR(p<0.001). Inpatient mortality was 20%, where 8% died within the first 24 hours. Overall survival was 73% at 30 days, 61% at 1 year, and 49% 5 years (Figure 1). Inpatient cost by treatment was $130,000±$194,000 for MED, $344,000±$344,000 for OPEN, and $3000,000±$500,000 for TEVAR(p<0.001). TEVAR was independently associated with improved survival compared to MED (HR:0.54,95% CI 0.36-0.81, p<0.003)(Table 1). Adjusted risk of complications was increased for OPEN(OR:4.3[CI:1.6-11]p=0.003) and Charlson score>3 (OR:5.9[ 3.8-9.3]p<0.001).
Conclusion:
Symptomatic type-B aortic dissection confers significant mortality and morbidity. Despite the small number of patients treated with TEVAR, the significantly improved outcomes relative to medical treatment warrants further study to determine its role in CTBAD management. 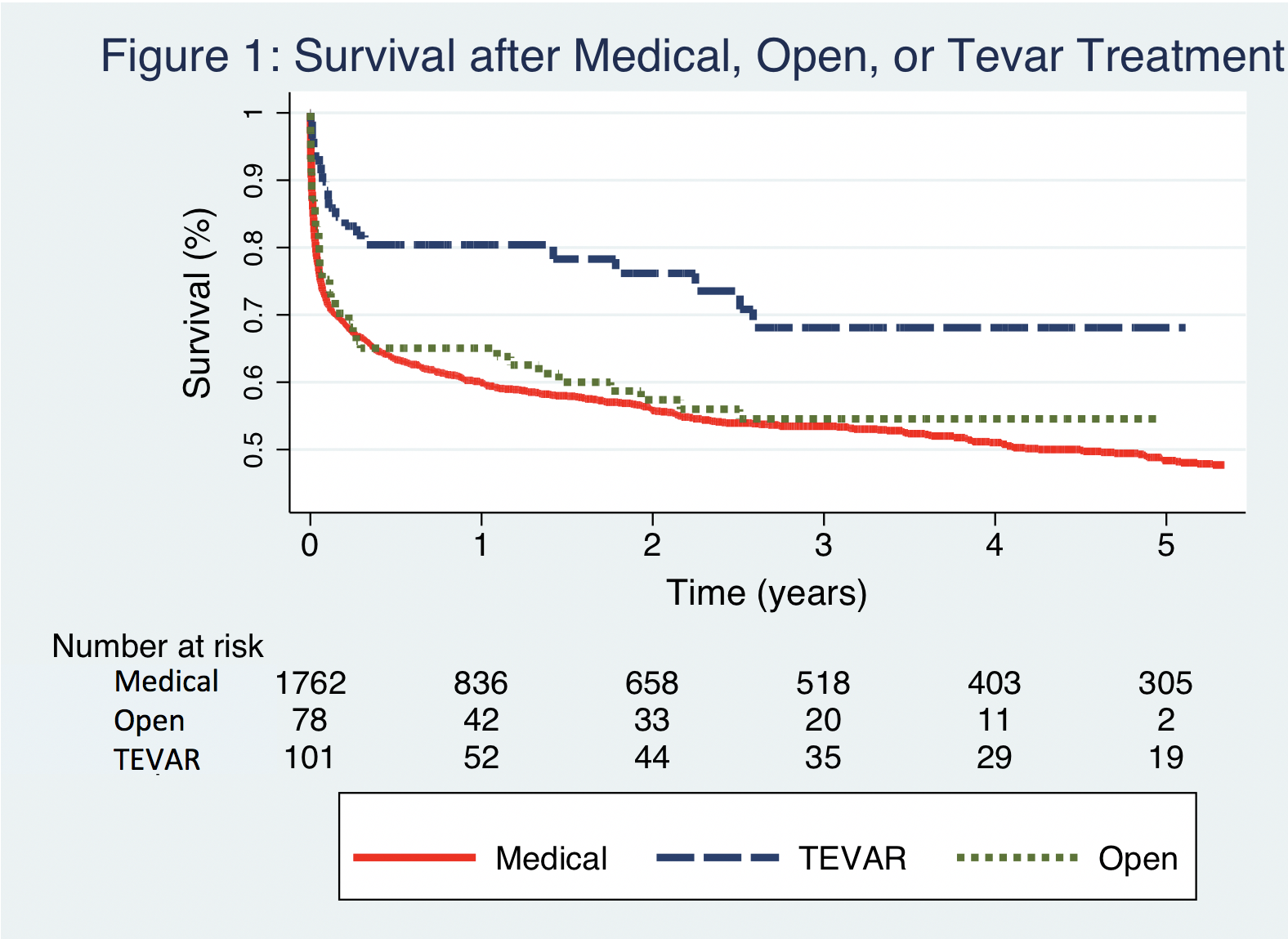
| Covariate | Hazards Ratio | 95% Confidence Interval | P-Value |
| TEVAR (Ref Medical Rx) | 0.54 | 0.36-0.81 | <0.01 |
| OPEN (Ref Medical Rx) | 1.1 | 0.81-1.41 | 0.64 |
| Age 50-59 (Ref <50) | 1.3 | 0.94-1.8 | 0.11 |
| Age 60-69 (Ref <50) | 1.9 | 1.5-2.4 | <0.01 |
| Age 70-79 (Ref <50) | 2.6 | 2.0-3.3 | <0.01 |
| Age >79 (Ref <50) | 3.7 | 2.9-4.7 | <0.01 |
| Acidosis | 1.3 | 1.1-1.5 | <0.01 |
| Shock | 1.6 | 1.3-1.9 | <0.01 |
| Charlson>3 | 1.3 | 1.1-1.5 | <0.01 |
Back to 2019 Abstracts
