Medicare Reimbursement for Endovascular Aortic Aneurysm Repair is Decreasing and Varies Substantially Across Centers
Spencer W. Trooboff, MD MBA1, Zachary Wanken, MD MS1, Barbara Gladders, MS2, Jesse Columbo, MD MS1, Bjoern Suckow, MD1, David Stone, MD1, Art Sedrakyan, MD PhD3, Philip Goodney, MD MS1.
1Dartmouth Hitchcock Medical Center, Hanover, NH, USA, 2The Dartmouth Institute for Health Policy and Clinical Practice, Hanover, NH, USA, 3Weill Cornell Medical College, New York City, NY, USA.
Objective
The cost of endovascular aortic aneurysm repair (EVR) has been evaluated in various studies. Most have been from a single center, or involved a clinical trial, and used administrative billing data to highlight the high initial cost of EVR. Real-world analyses of reimbursement for EVR at a national level are lacking. We sought to characterize variation in reimbursement for index EVR hospitalizations among Medicare beneficiaries.
Methods
We linked Medicare claims to clinical registry data from the Vascular Quality Initiative (VQI) for patients undergoing EVR from 2003-2015. The analytic cohort was limited to patients who were fully covered by Medicare Parts A&B fee-for-service in the year of their operation. Index hospitalization reimbursement was determined using the amount paid by Medicare for inpatient hospital and professional fees. We performed descriptive analyses of reimbursement over time and by complication status and type. We then conducted a sub-analysis of reimbursement variation among uncomplicated patients at the level of VQI-participating centers. Any center performing ≤10 EVR procedures was suppressed.
Results
We identified 10,156 Medicare-VQI matched patients undergoing EVR during the study period. There were 108 EVR procedures identified in 2003 which rose to 1,746 procedures by 2015. Average reimbursements for EVR increased at an annualized rate of 3.6% from $22,612 in 2003 to $28,925 in 2010. Reimbursement then declined at 1.8% annually from 2010-2015. The overall mean payment for uncomplicated EVR was $25,766 ± $10,502. For patients experiencing a complication (n=884, 8.7%), the mean payment for index EVR was $45,542 ± $36,669. The complications associated with the highest payments on average were intestinal ischemia ($68,602), respiratory failure ($63,039), and surgical site infections ($61,762). On sub-analysis of patients who underwent uncomplicated EVR at one of 132 VQI-participating centers, mean center-level reimbursement ranged from $17,984 to $42,142 - Figure 1.
Conclusions
The occurrence of postoperative complications understandably corresponds with higher reimbursement levels for index EVR. Yet, even among uncomplicated EVR procedures, there is more than two-fold variation in Medicare payments across VQI-participating centers. Further study is needed to define patient and procedure characteristics as well as diagnostic coding patterns associated with this potentially unwarranted variation. 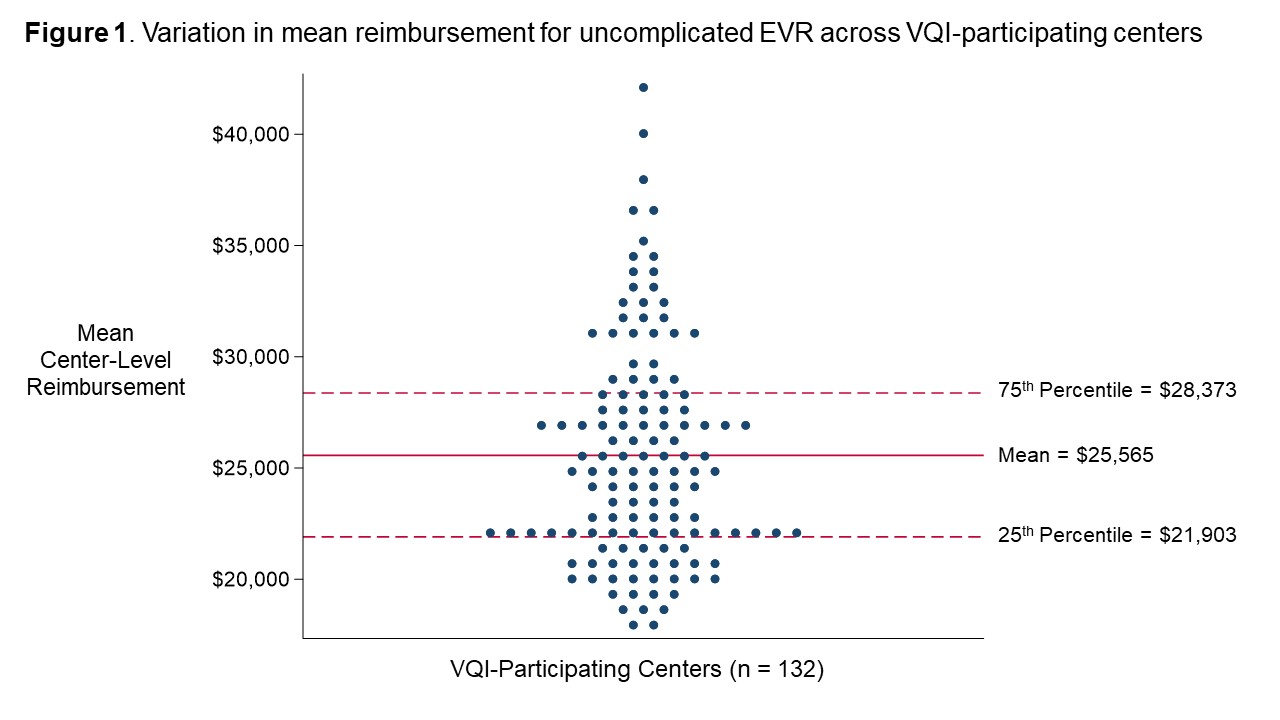
Back to 2019 Abstracts
