Long term outcome of Thoracofemoral Bypass
Indrani Sen, Manju Kalra, Thomas C. Bower, Jill K. Johnstone, Randall R. DeMartino, Fahad Shuja, Gustavo S. Oderich, Peter Gloviczki.
Mayo clinic, Rochester, MN, USA.
Introduction The aim of this study was to evaluate early and late outcomes of descending thoracic aorto-iliac /femoral (DTAI/F) bypass. Methods Data from consecutive patients undergoing DTAI/F bypass between 1980 and 2018 were retrospectively reviewed. Clinical features, radiographic findings, operative details and morbidity were recorded. Primary end points were mortality, graft patency and limb salvage. Results Of 6800 interventions for aortoiliac occlusive disease; 35 patients (19male, 16 female; median age 58yrs) underwent DTAI/F bypass because of failed prior aortoiliac/femoral (n=15; 1 infection) or axillofemoral (n=1) bypass; hostile abdomen from prior non-aortic surgery (n=3), radiation arteritis (n=7); or suprarenal/paravisceral stenosis (n=9). Clinical indications were lower extremity claudication (n=29) or renovascular hypertension (n=6). Inflow was from the descending thoracic aorta in 30 and supraceliac aorta in 5. Outflow was to bilateral femoral (fem-fem cross over) in 22, ipsilateral femoral in 5 and infrarenal aorta in 8. The conduit used was Dacron (33; 5 rifampin soaked) or PTFE (n=2). Mesenteric/ renal bypasses were performed in 7 patients (4 midaortic syndrome, 4 atherosclerosis, 1 infection). There was no 30-day/ in hospital mortality/ amputation; complications occurred in 4/35 (11%) patients (temporary renal insufficiency based on RIFLE criteria in 3, atrial fibrillation in 1, pneumonia in 2. There was no correlation of femorofemoral limb thrombosis with preop risk factors. One early graft excision was performed for infection due to inadvertent tunneling through bowel. Median length of stay was 8 (3-66) days. Median clinical follow up was 5 years (1 month-27 years). Four patients were lost from any follow up. Median imaging follow up was 3 years (1 month- 22 years). On Kaplan Meier analysis (Figure 1), primary and secondary patency for the DTAI/F at 10 years were 92%; for fem-fem crossover limbs were 65% and 80%, and survival 90% respectively. Four pts died from non- aortic causes. No patient required amputation or subsequent infra-inguinal reconstruction. Conclusions: Descending thoracic aorto-iliac /femoral bypass is associated with low operative mortality / morbidity, and excellent long-term durability. DTAI/F bypass remains a viable option for lower extremity revascularization in patients with failed open / endovascular aortoiliac reconstruction or high aortic lesions. 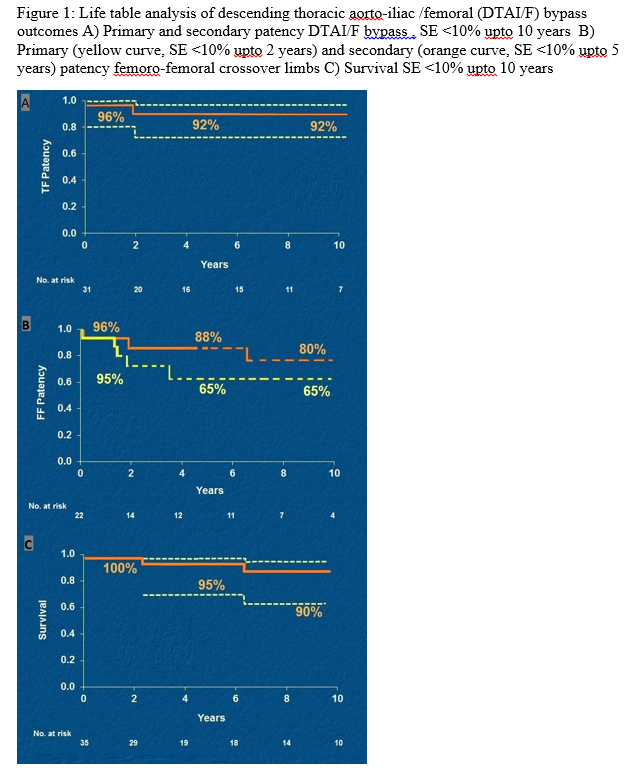
Back to 2019 Abstracts
