Validation of a Preoperative Prediction Model for Mortality within One Year after Endovascular Aortic Aneurysm Repair of Intact Aneurysms
Salvatore T. Scali, M.D.1, Adam W. Beck, M.D.2, Mohammed Eslami, M.D., M.S.3, Marc Schermerhorn, M.D.4, Jack L. Cronenwett, M.D.1, Michael Singh, M.D.3, Alfio Carroccio, M.D.5, Dan Neal, M.S.1.
1University of Florida-Gainesville, Gainesville, FL, USA, 2University of Alabama-Birmingham, Birmingham, AL, USA, 3University of Pittsburgh, Pittsburgh, PA, USA, 4Beth Israel Deaconess Medical Center, Boston, MA, USA, 5Lenox Hill Hospital, New York City, NY, USA.
OBJECTIVES: Most would agree that at least 1-year survival is necessary after intact abdominal aortic aneurysm(AAA) repair to appropriately justify the cost and risk of the procedure. No validated clinical decision instruments exist to predict survival after endovascular aneurysm repair(EVAR) beyond the perioperative period. The purpose of this analysis was to create a preoperative prediction model for 1-year mortality after EVAR for intact AAA in the Society for Vascular Surgery Vascular Quality Initiative(SVS-VQI).
METHODS: All intact EVARs from 2011-15 were randomly divided into training (N=17,836) and validation(N=2,500) datasets, and 31 preoperative candidate predictors were identified. A logistic regression model for 1-year mortality was created, and bootstrapped step-wise variable elimination was used to identify a best subset of predictors. The final model was internally validated by bootstrapping the area under the curve(AUC) and the calibration slope and intercept, and externally validated by application to the validation dataset.
RESULTS: After elective and non-elective(symptomatic/intact) EVAR, 1-year mortality was: 5.5%(n=900/16,411) and 11.4%(n=162/1425), respectively. The mean probability of 1-year mortality in the training set was 6.0%(n=1062) and 5.7%(n=143) in the validation cohort(p=.12). Significant preoperative predictors of 1-year mortality included: chronic obstructive pulmonary disease, age, preoperative renal insufficiency(creatinine≥1.8mg/dL and/or hemodialysis), ejection fraction<50%, transfer status, BMI<24kg/m2, preoperative beta blocker exposure, larger AAA diameter, and lower admission hemoglobin(mg/dL). Preoperative statin use was found to be protective. The bias-corrected AUC=.759(Hosmer-Lemeshow goodness of fit p-value= .36, calibration intercept= -0.003 and slope= .999). This model was externally validated by application to the validation dataset[AUC = .724;95% CI=.676, .768, calibration intercept= 0.0009 and slope= .970], which was in excellent agreement with the original dataset bias-corrected AUC. Notably, ~27.5%(N=4902) had ≥ 4 risk factors with a predicted 1-year post-EVAR mortality risk of 10-22% despite 33.2% of these subjects having AAA diameters below recommended treatment guideline minimum thresholds(Figure).
CONCLUSIONS: This validated preoperative prediction model for 1-year mortality identifies patients less likely to benefit from EVAR. Appropriateness of intact AAA EVAR care delivery can be improved by utilization of this clinical-decision aid to determine which high-risk patients have lower probability of mortality within the first postoperative year relative to their predicted annualized rupture risk. 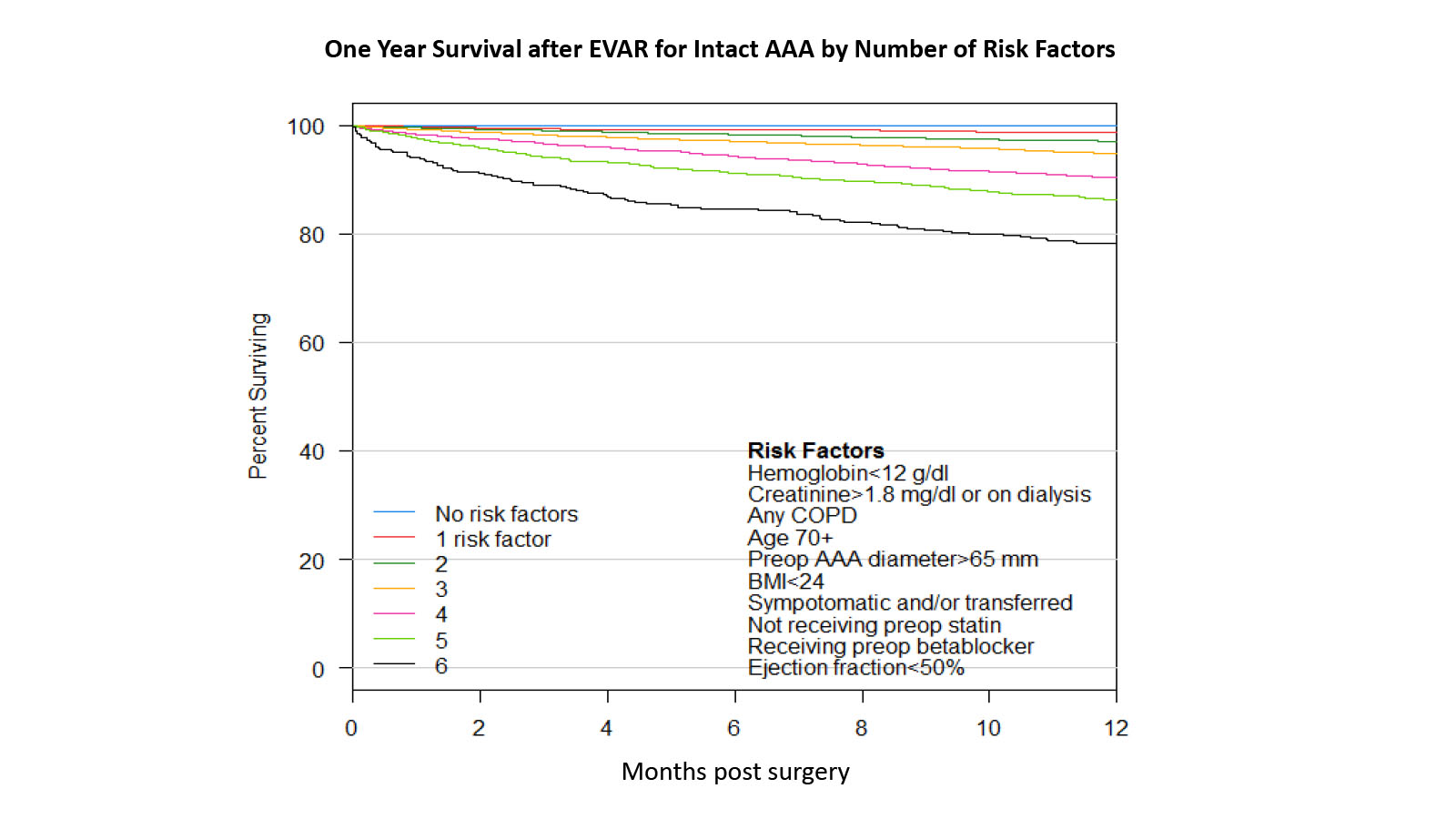
Back to 2019 Abstracts
