Predictors of Ambulatory Status at One-Year Following Major Lower Extremity Amputation
Kyle R. Diamond, MD1, Grace J. Wang, MD, MSCE2, Allison S. Wyman, MS1, Edward J. Arous, MD, MPH1, Dejah R. Judelson, MD1, Francesco Aiello, MD1, Andres Schanzer, MD1, Jessica P. Simons, MD, MPH1.
1University of Massachusetts Medical School, Worcester, MA, USA, 2Division of Vascular Surgery and Endovascular Therapy, Hospital of The University of Pennsylvania, Philadelphia, PA, USA.
OBJECTIVES: Nearly 60,000 major lower extremity amputations (AKA/BKA) are performed annually in the United States. Once the decision is made that AKA/BKA is necessary, the primary goal shifts to maintaining physical function. We sought to create a simple risk score for predicting ambulation at one-year following AKA/BKA.
METHODS: We queried the Vascular Quality Initiative amputation database for patients who underwent above-knee (AKA) or below-knee (BKA) amputation (2013-2018). We excluded patients who were wheelchair- or bed-bound preoperatively and those without information on 1-year ambulatory status. The primary endpoint was ambulation at one year, defined as either independent or with assistance. The cohort was divided into an 80% derivation set and a 20% validation set. Using the derivation set, a multivariable model identified preoperatively-available independent predictors of 1-year ambulation. The beta coefficients were rounded to create an integer-based risk score. Scores were calculated and patients were assigned to risk groups according to the chance of being ambulatory at one year (low chance, medium chance, and high chance). Internal validation was performed by applying the risk score to the validation set. Discrimination and calibration were assessed with receiver operator characteristic curves and Hosmer-Lemeshow goodness-of-fit testing, respectively.
RESULTS: Of 8725 AKA/BKA, 2055 met inclusion criteria (exclusions: 2644 patients nonambulatory prior to amputation, 3753 missing 1-year follow-up ambulatory status). The majority (n=1366, 66%) were BKAs. The most common indication was chronic limb threatening ischemia (47%, ischemic tissue loss; 9%, ischemic rest pain; 35%, infection/neuropathic; 9%, acute limb ischemia). Ambulation at one year was higher for BKA than AKA (n=921, 67%, versus n=343, 50%, p<.0001). In the final prediction model, contralateral BKA/AKA was the strongest predictor of NON-ambulation. The score provided reasonable discrimination (c-statistic=0.65) and was well calibrated (Hosmer-Lemeshow p=.24).
CONCLUSIONS: In this real-world dataset, the majority (62%) of patients who were ambulatory before major amputation remained ambulatory at one year postoperatively. An integer-based risk score can be used to stratify patients according to chance of ambulation at one year after major amputation and may be useful for preoperative patient counseling. 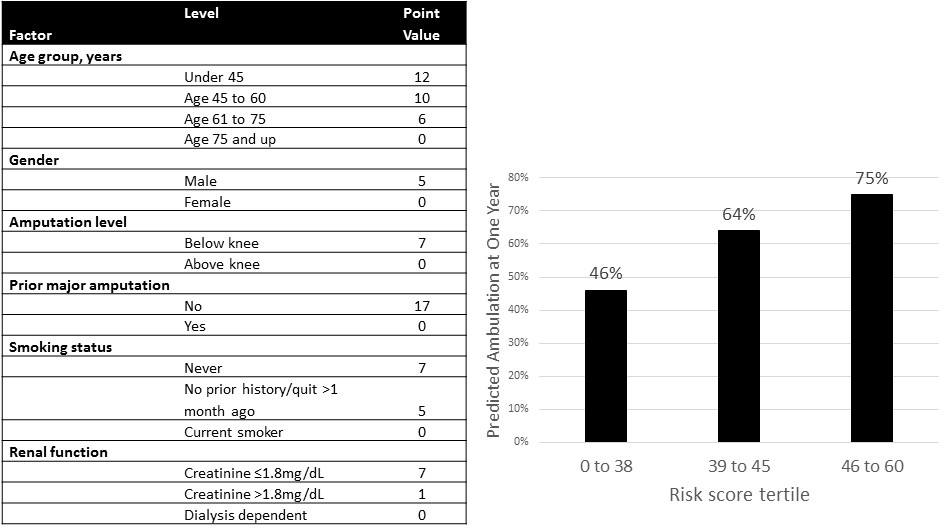
Back to 2019 Abstracts
