Open Repair of a Complicated Type IA Endoleak
Christine Dubberke, MD, Mohammed Moursi, MD.
UAMS, Little Rock, AR, USA.
DEMOGRAPHICS
82 yo WM with history of chronic ITP, splenectomy, COPD, and EVAR.
HISTORY
5.8 cm AAA with a 28 X 10 mm neck and dilatation to the diaphragm that was initially repaired with a 36mm graft on 4/11/16. He had a persistent type 1a endoleak and unsuccessful palmaz stent placement on 5/12/16. He subsequently underwent direct sac glue embolization on 6/13/2016 and 7/15/16 for his persistent type 1A endoleak. CTAs on 10/11/16 and 11/17/17 showed no evidence of residual endoleak, however he had interval sac growth to 6.5 cm, and was then lost to follow up. He presented as a transfer from an outside hospital on 5/29/18 with a non-contrast CT that showed a ruptured AAA into the left retroperitoneum. Although patient was elderly, he was functional, lived independently, and desired repair.
PLAN
A bilateral subcostal incision was used for supraceliac aortic control. The aorta was opened and the endoleak was identified by active bleeding from the superior, lateral aspect of the endograft-aorta interface. This leak was closed with two 3-0 prolene sutures in a figure of 8 fashion that buttressed the graft to the aneurysm sac. The sac was closed and the patient made a full recovery. He was discharged on POD#5, and is currently doing well.
DISCUSSION
Type Ia endoleak incidence is 3 -21% and should be repaired at discovery. Initial approach is to re-balloon the fixation site, followed by placement of aortic cuffs, a balloon-expandable stent, or endostaples. Refractory cases may require glue or coil deposition within the sac, chimney technique, or a fenestrated device. Up to 5% of EVARs require open repair with complete or partial endograft removal and are associated with significant morbidity and mortality. Emergent conversions have a mortality up to 22%. In this case report, the patient was thought to be unfit for open elective repair, thus multiple endovascular modalities were used unsuccessfully for endoleak. Eventually, he presented with a rupture necessitating emergent open repair, which was accomplished with 2 stitches that obliterated the endoleak from within the aneurysm. He recovered from the surgery and is doing well.
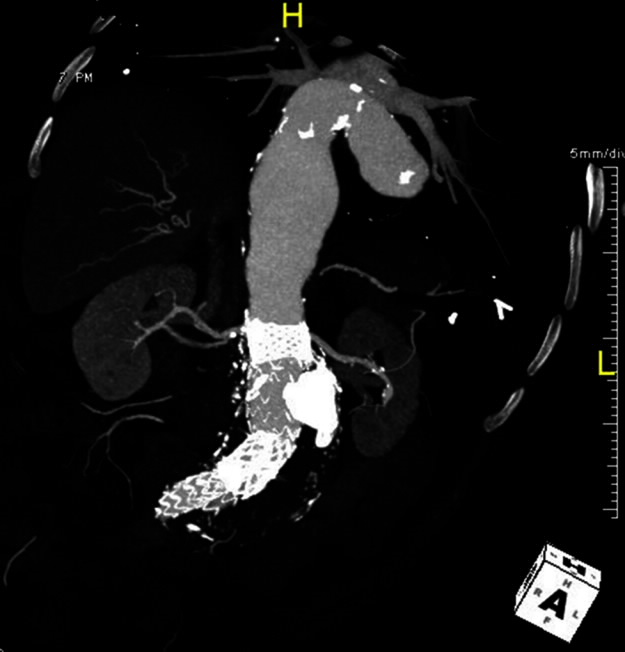
CTA from 11/17/17
Back to 2019 ePosters
