Raising the Bar for Appropriateness in the Care of Patients with Peripheral Artery Disease
Cassius I. Ochoa Chaar, MD1, Arash Fereydooni2, Peter F. Lawrence, MD3, Alan Dardik, MD, PhD1.
1. Section of Vascular Surgery, Department of Surgery, Yale University School of Medicine, New Haven, CT, USA, 2Yale School of Medicine, New Haven, CT, USA, 3Division of Vascular and Endovascular Surgery, David Geffen School of Medicine at the University of California, Lost Angeles, CA, USA.
OBJECTIVES: Advances in endovascular therapy have exponentially increased the number of procedures performed for peripheral artery disease (PAD), but public concerns of overuse have placed the vascular community under scrutiny. Appropriateness of care has thus become the focus of several professional societies, but literature on the topic is limited. This report describes 2 cases of inappropriate care and highlights opportunities for improvement.
METHODS: The medical records of 2 patients seen for second opinion were reviewed.
RESULTS: The first patient is a 57-year-old with known PAD. He presented 3 years prior with rest pain in the left foot and underwent left femoral endarterectomy and bilateral kissing iliac stents with resolution of symptoms. He then complained of knee pain when walking, right worse than left, after 10-15 steps. Ankle brachial index (ABI) on the right was 0.76, but no intervention was offered. He sought second opinion with another provider who performed recanalization of the right superficial femoral artery (SFA). Follow-up ultrasound showed patent SFA. As his symptoms persisted, the patient returned to our care and was referred to orthopedic surgery for evaluation of osteoarthritis. The second patient is an 84-year-old woman on hemodialysis who was evaluated for right foot rest pain and superficial toe ulceration. She underwent bilateral kissing iliac stents and was found to have a right SFA occlusion. She underwent a second diagnostic angiogram for continued foot pain, which determined the pain was not vascular in etiology. She was seen by our service for second opinion and ABI was performed for the first time in her care and it demonstrated a right toe pressure of zero. She underwent a challenging percutaneous recanalization of the right SFA (Figure 1 A, C), as well as stenting of the above knee popliteal artery (Figure 1B, D) via left brachial artery approach. Rest pain resolved; her ulcer healed; and the toe pressure increased to 60mmHg. She has had no recurrence of symptoms after 6 months.
CONCLUSIONS: The evaluation and treatment of patients with PAD requires thorough history taking, physical examination, and appropriate imaging. Guidelines for appropriateness of care in PAD may limit unnecessary procedures. 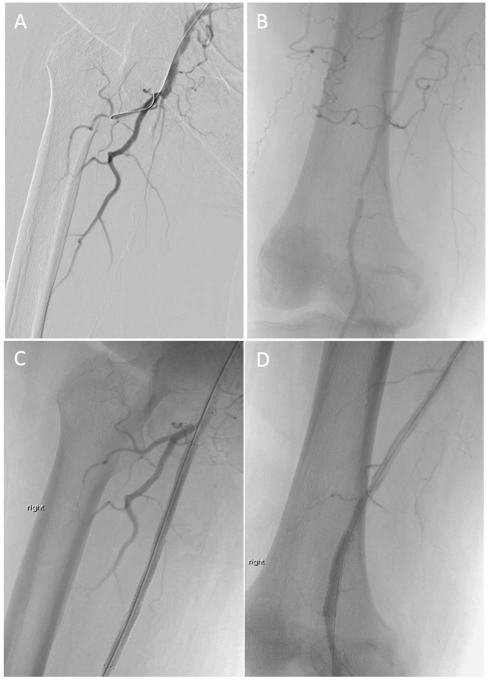
Back to 2019 ePosters
