Open and Endovascular Repair of 2 Ureteral Arterial Fisutulas
Cheryl Richie, M.D., Brent Hillard, M.D., Jon Demos, M.D., David Minion, M.D., Sam Tyagi, M.D..
University of Kentucky, Lexington, KY, USA.
DEMOGRAPHICS and HiSTORY: First, a 78 year old male with a history of a radical cystoprostatectomy with ileal conduit for bladder cancer and long-term left ureteral stenting, presented to the ED with urosepsis. Similarly, a 68 year old female with a long-standing left ureteral stent for the treatment of stricture following pelvic radiation for rectal cancer, presented to the ED with hematuria. During stent exchange in both patients, brisk, pulsatile bleeding was noted. In both patients, expeditious ureteral stent exchange resulted in temporary hemorrhage control.
PLAN and TREATMENT: The 78 year old patient underwent open repair via a transabdominal incision, the ureter, fistula, and iliac vessels were exposed. The ureter was ultimately resected by urology with plans for a permanent percutaneous nephrostomy tube. The external iliac artery underwent primary repair.
The 68 year old patient was deemed unsuitable for open surgery secondary to her severely diminished functional status. Based on preoperative CTA, two locations for the fistula were possible, one at the external iliac and one at the hypogastric artery. Two stent grafts were placed via a retrograde femoral access, covering both of these sites and patient was placed on long-term suppressive antibiotic therapy.
DISCUSSION: Ureteroiliac fistulas are a unique and rare disease process which requires a dual specialty surgical approach. Here we present the case of two patients who developed an ureteroiliac fistula as a complication of long-term indwelling ureteral stents. Ureteroiliac fistulas present several challenges for patients and providers. Open surgery is almost always complicated by redo or radiated operative fields and endovascular approaches carry risk of graft infection. Here we demonstrate successful treatment of this condition with both an open and endovascular approach. 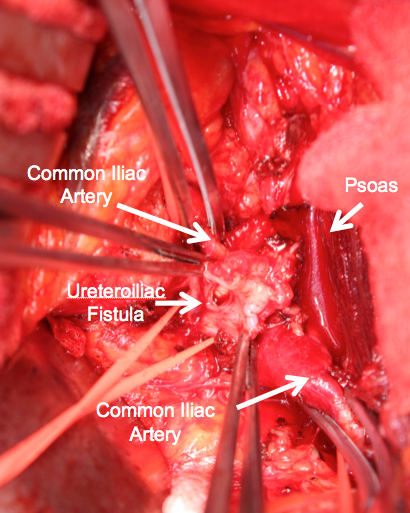
Back to 2019 ePosters
