Occluded Internal Carotid Artery Stent as Source of Carotid Stump Syndrome
Avianne P. Bunnell, MD, Thomas E. Brothers, MD.
Medical University of South Carolina, Charleston, SC, USA.
DEMOGRAPHICS
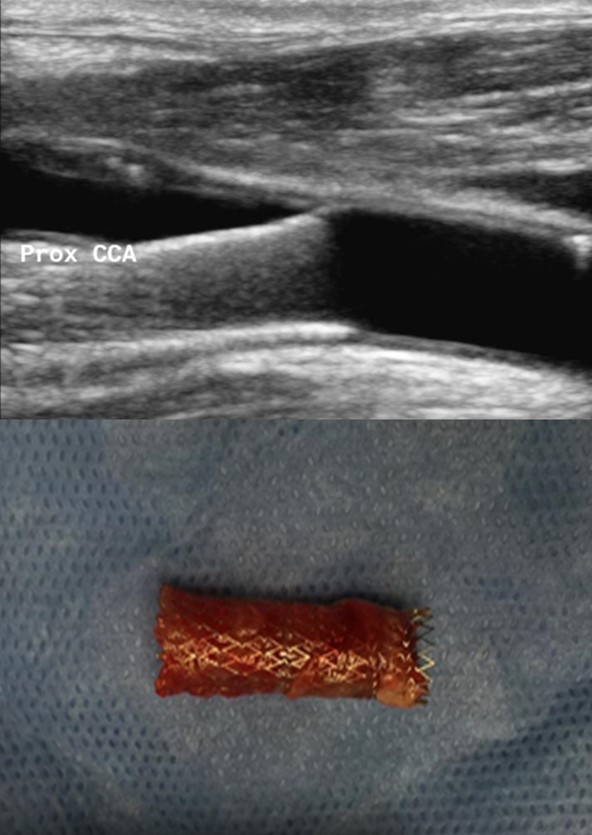
A 62-year-old man presented with symptoms of intermittent right eye vision loss two years after percutaneous carotid bare-metal stent treatment for symptomatic internal carotid stenosis due to atherosclerotic disease. Carotid duplex ultrasound demonstrated a distally occluded stent traversing the common carotid artery
HISTORY
The patient had previously suffered a right middle cerebral artery territory stroke at age 60, almost three years prior to presentation. Upon evaluation years later, this was believed to be due to critical stenosis of the right internal carotid artery. Because the patient also had a history of right neck radiation exposure, previous neck dissection for excision of tonsillar cancer, and known contralateral vocal cord paralysis requiring prolonged intubation and tracheostomy after recent left carotid endarterectomy, also for symptomatic stenosis, his right-sided disease was treated with a carotid stent. Additional medical problems included hyperlipidemia, hypertension, hypothyroidism, gastroesophageal reflux disease, iron deficiency anemia, and post-traumatic stress disorder.
PLAN
Treatment consisted of open right carotid exploration with care to avoid cranial nerve injury, extraction of the stent, limited endarterectomy of the external carotid artery, and flush ligation of the internal carotid artery. Operative findings suggested that flow to the external carotid had to pass through the nearly occluded interstices of the proximal portion of the stent lying obliquely in the carotid bulb. The patient tolerated the procedure well and has been followed out to 33 months with no further symptoms of retinal or cerebral ischemic events.
DISCUSSION
Carotid stump syndrome occurs rarely after internal carotid artery occlusion. It has been associated with increased risk of ongoing embolic events leading to ischemia via collateral pathways from the external carotid artery. The standard treatment described has involved open carotid exploration with flush ligation of the internal carotid artery. Current literature has not well described the management of stump syndrome after carotid artery stenting. With the increasing implementation of the percutaneous arterial stenting for carotid artery disease and the inherent risk of stent occlusion, contribution of an occluded stent to the development of symptoms of carotid stump syndrome should be considered.
Back to 2019 ePosters
