Endovascular Management of Non-Salmonella Infected Aortic Aneurysms
Nii-Kabu Kabutey, MD, William Duong, MD, Samuel Chen, MD, Bima Joseph, Isabella Kuo, MD, Carlos E. Donayre, MD, Roy M. Fujitani, MD.
University of California, Irvine, Orange, CA
Objectives: Infected aortic aneurysms (IAA) are a rare condition that can rapidly progress to rupture and death. Surgical mortality has been reported to be between 13-40%. Treatment for IAA has been surgical resection for source control, followed by aortic reconstruction or extra-anatomic bypass. Endovascular repair has been reported as a viable option for bridging patients to definitive open repair. We reviewed our institution's experience with IAA managed by endovascular stent graft repair.
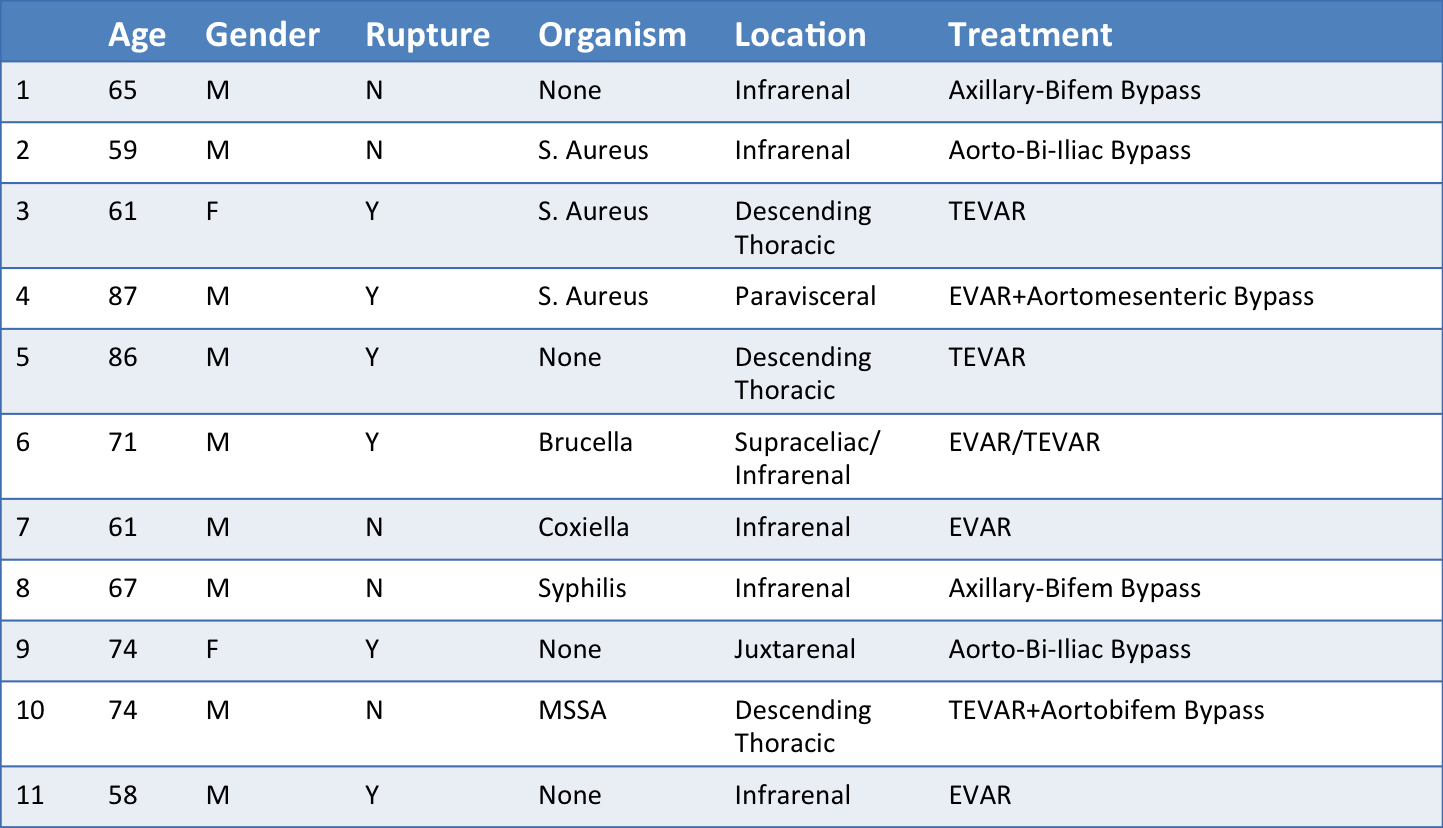
Methods: We performed a retrospective review of all cases of IAA treated at our institution from 2007-2017. Patient demographics, symptomatology, anatomical characteristics, microbial organisms and operations performed, were all recorded and analyzed.
Results: Eleven subjects were found at our institution to have been treated for IAA during the study period. 81% (9/11) of the patients were male, with a mean age of 69. The anatomic locations of the infection were thoracic aorta 27% (3/11), abdominal aorta 54% (6/11), as well as concomitant lesions of the thoracic and abdominal aorta 18% (2/11). Eight patients were treated solely with endovascular repair. 55% (6/11) of the patients presented with aortic rupture. Two patients were treated with extra-anatomic bypass, two patients were treated with in-line reconstruction, and two patients were treated with hybrid open and endovascular repair. Staphylococcus infection was present in the majority of cases 36% (4/11), other organisms included Brucella 9% (1/11), Coxiella 9% (1/11), Salmonella 9% (1/11) and Syphilis 9% (1/11). Seven out of 8 endovascular repair patients were for non-Salmonella infection of the aorta. There was one endovascular death 9% (1/11) and there was one intraoperative hybrid death 9% (1/11). All endovascular repair cases were placed on long-term suppressive antibiotic therapy. Average follow-up time was approximately 2 years. There have been no endovascular stent graft infections so far that have required graft extraction.
Conclusions: Endovascular management of IAA can be a viable alternative to open surgery. We did not find a large percentage of infection-related complications or death associated with endovascular repair. Long-term follow-up is required to determine whether endovascular management can be a durable therapy for non-Salmonella aortic infections.
Back to 2019 ePosters
