Open Peripheral Revascularization for Limb Salvage After Failed Peripheral Angioplasty and Recommended Amputation for a Non-Healing Diabetic Ulcer
Joel L. Ramirez, BS, Devin S. Zarkowsky, MD, Alexander M. Reyzelman, DPM, Michael S. Conte, MD.
University of California, San Francisco, San Francisco, CA, USA.
DEMOGRAPHICS: A 53-year-old man from Guatemala with a history of CAD, HLD, CKD, and DM1 presented with a worsening right foot ulcer (WIfI Stage 3) for eight months (Figure A).
HISTORY: He previously underwent a right fifth metatarsophalangeal debridement in Guatemala for suspected hyperkeratosis. After the debridement, the wound enlarged and became necrotic. He then presented to a robust community vascular practice in the United States, underwent a lower extremity diagnostic angiogram without intervention, and was offered a below-knee amputation. Three months ago, he sought out another opinion at an academic hospital in the United States where he underwent a right tibial artery angioplasty. He continued to have progressive wound necrosis and, once again, was advised to undergo a below-knee amputation prior to presenting to our institution.
PLAN: Non-invasive physiologic testing demonstrated a right ABI of 0.79 with a toe pressure of 41 mmHg. He underwent wound debridement and bone biopsy, which returned with nafcillin-sensitive Enterococcus and Staphylococcus Aureus osteomyelitis. A diagnostic right lower extremity angiogram demonstrated distal occlusion of the anterior peroneal artery with reconstitution of the dorsalis pedis artery on the foot (Figure B). He then underwent a right below-knee popliteal artery to dorsalis pedis artery bypass using non-reversed autogenous greater saphenous vein followed by a right partial fifth ray resection (Figure C). Postoperatively, the patientís toe pressure improved to 95 mmHg. He was discharged on POD4 with a wound vacuum and a two-week course of amoxicillin-clavulanate. Follow-up seven weeks after surgery demonstrated an adequately healing wound (Figure D).
DISCUSSION: Critical limb ischemia challenges even experienced surgeons at well-equipped medical centers, as evidenced by this patientís Pan-American medical tour. Endovascular approaches to the distal tibial vessels via either anterograde or - with increasing popularity - retrograde approaches have not demonstrated the same efficacy and durability as pedal bypass. However, the disparity in technical skill required to perform each procedure has anecdotally lead to our practice encountering several patients, including this one, who had revascularization attempted with an endovascular-only approach before receiving a recommendation for amputation. This case highlights the profound impact a multidisciplinary limb preservation practice can have. 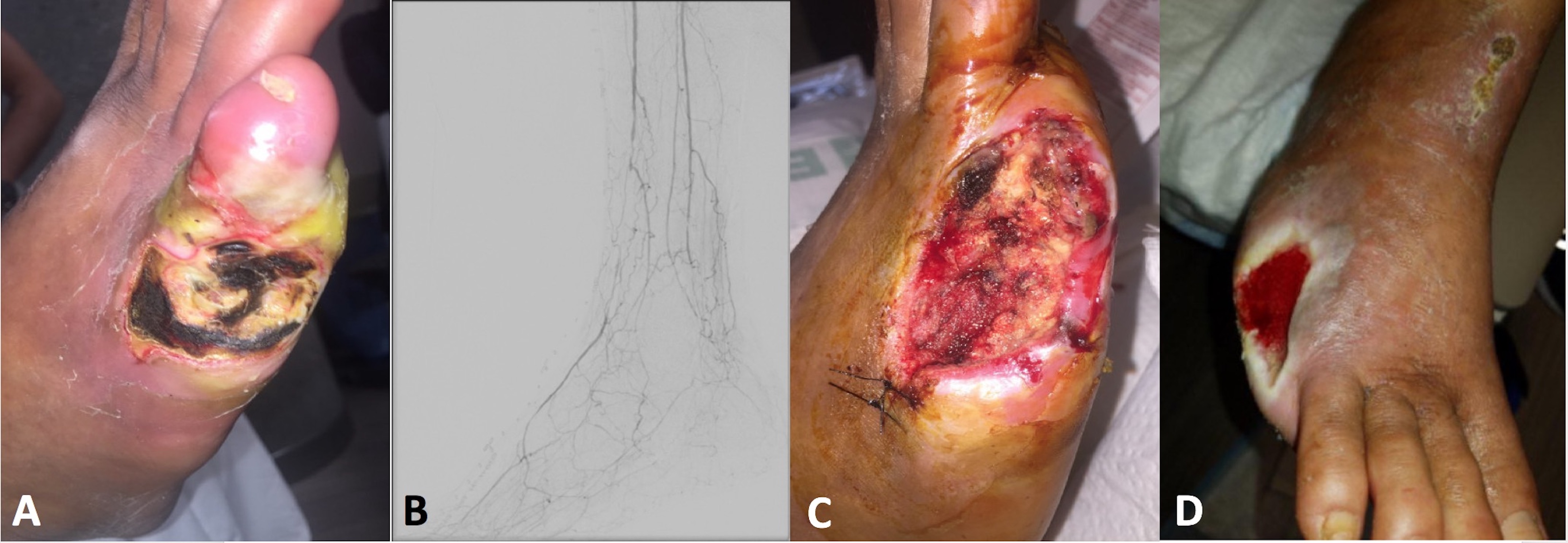
Back to 2019 ePosters
