Two-Stage Hybrid Repair of a Thoracic Aortic Aneurysm with Aortobronchial Fistula After Open Repair for Aortic Coarctation and TEVAR
Joel L. Ramirez, BS, Devin S. Zarkowsky, MD, Charles M. Eichler, MD, Michael S. Conte, MD.
University of California, San Francisco, San Francisco, CA, USA.
DEMOGRAPHICS: A 66-year-old man with a history of HTN, HLD, ESRD, and open repair of aortic coarctation 30 years ago, which was complicated by a pseudoaneurysm that was treated with a TEVAR 14 years ago, presented to an OSH with three weeks of hemoptysis.
HISTORY: The patientís TEVAR had a type 1A endoleak identified four years ago that communicated with a thoracic aortic aneurysm (TAA). CT scan at presentation demonstrated a 6.0 x 7.3 cm descending TAA and a persistent endoleak with gas in the aneurysm sac but no active extravasation, suggesting the presence of an aortobronchial fistula or gas-forming bacteria (Figure A). Given his surgical history, he was deemed too high-risk for surgery at his original treating institution when the endoleak was initially identified and after he developed hemoptysis.
PLAN: At our institution, he received a two-stage hybrid repair procedure. First, he underwent an open aortic arch debranching, which included an ascending aorta to innominate artery bypass with a jump graft to the left common carotid artery and a left common carotid artery to left axillary artery bypass. Second, his previous TEVAR was extended to Zone 0 and the left subclavian artery was coil embolized, which successfully excluded the aneurysm and endoleak (Figure B). His postoperative course was complicated by a TIA. He was discharged on lifelong intravenous antibiotics on POD 20. He is now three months postoperative and recovering well.
DISCUSSION: Durability and surveillance are key concepts differentiating the endovascular era from purely open surgery. While reinterventions are often viewed as technical failures, a significant proportion of patients require adjunctive treatments to seal their aneurysm, suggesting that surveillance and retreatment are imperative rather than optional. In this case, we encountered a patient with a type 1A endoleak and associated mycotic aneurysm, a very difficult problem to treat, particularly in a fragile person with multiple comorbidities and an extensive surgical history. Ominous herald bleeding expedited our treatment, and we believe accepting the imposition of lifelong antibiotics appropriately balanced the benefit of this procedure against the morbidity associated with surveillance-only or a definitive reconstruction to unaffected tissue. 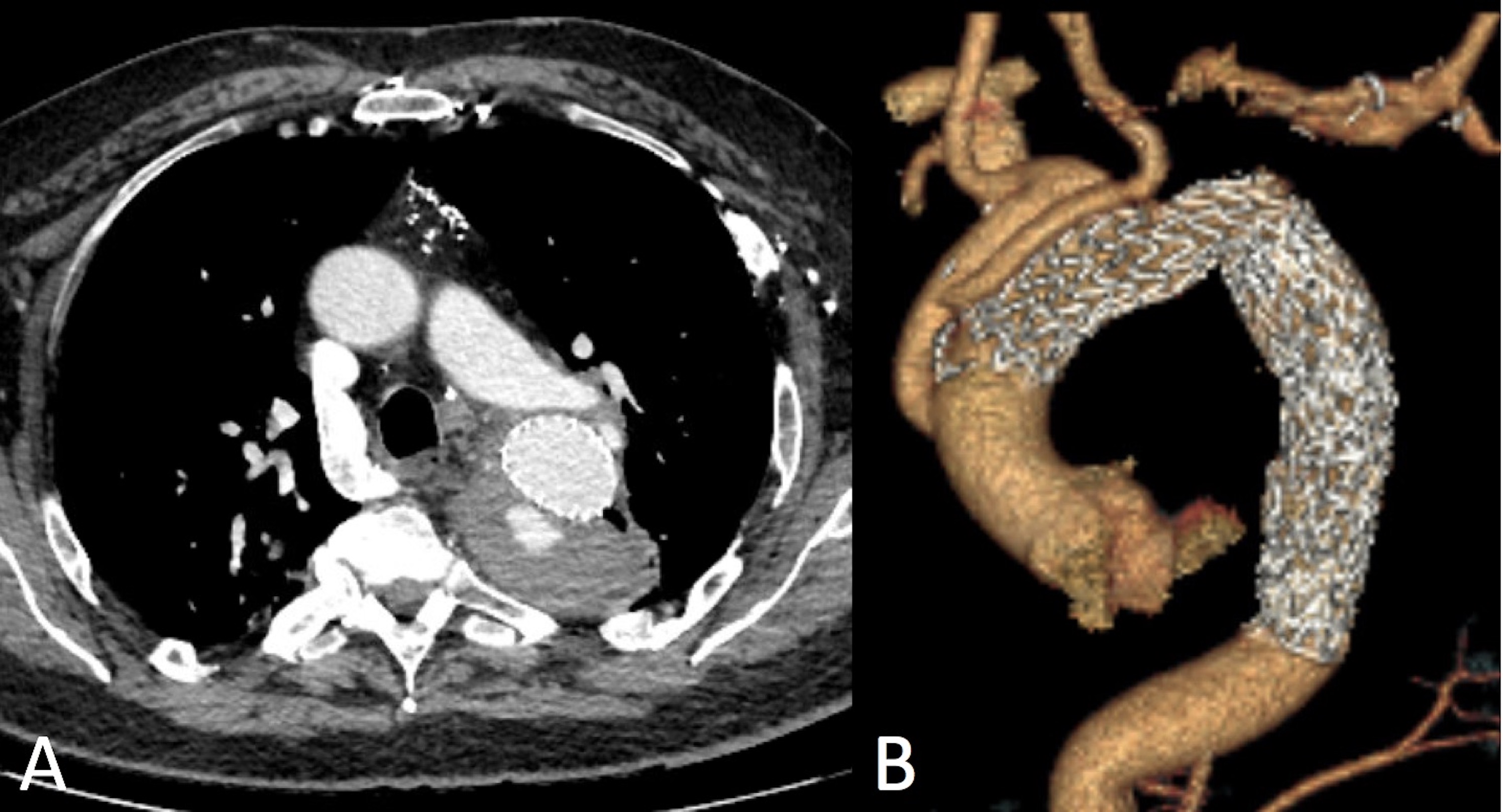
Back to 2019 ePosters
