Understanding Hepatic Artery Anatomy And Possible Anatomic Variables Through Open Treatment Of A Complex Hepatic Artery Aneurysm
Anthony C. Feghali, MD, Paul DiMuzio, MD.
Thomas Jefferson University, Philadelphia, PA, USA.
DEMOGRAPHICS:74 yo male presents with incidentally found 2.4cm hepatic artery aneurysm on CT being followed for history of bladder cancer. CT in 2014 measured the aneurysm 1.7cm.
HISTORY: Significant history includes treated bladder cancer. CTA revealed a common hepatic artery aneurysm extending to its origin on the aorta and involving the gastroduodenal artery (GDA) into the proper hepatic.
PLAN: Given the CT findings we performed an angiogram to see if there was a role for endovascular treatment. On angio the aneurysm appeared to only involve a short segment of the hepatic artery. On imaging of the GDA, there was a branch going into the left lobe of the liver. Given these complex findings we planned for an open repair. We considered an aortic to hepatic artery bypass or interposition grafting. We were prepared to reimplant the GDA if it provided flow into the left lobe of the liver.
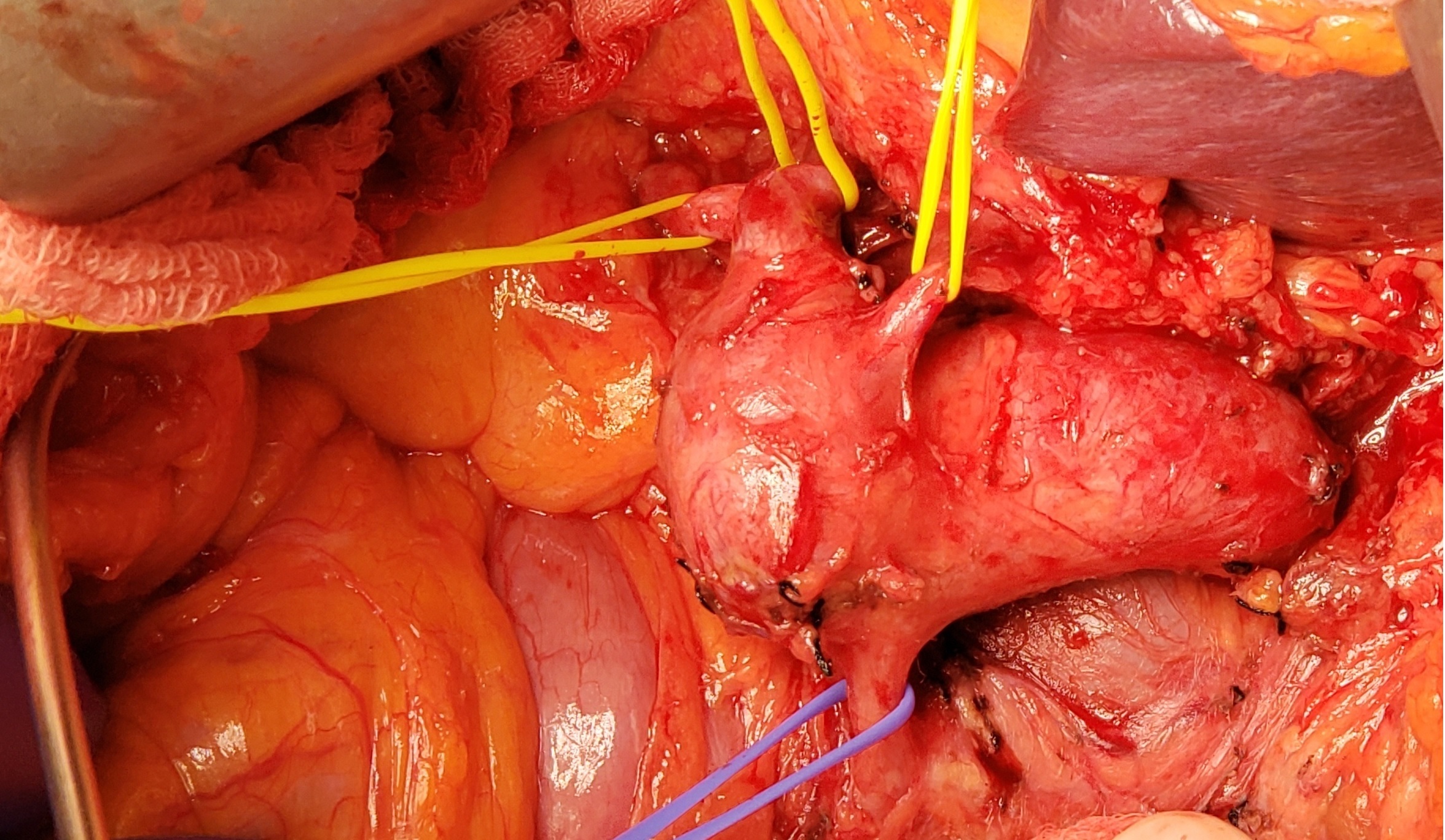
DISCUSSION: We explored through a midline laparotomy. We entered the lesser sac and dissected out the large hepatic artery aneurysm. We mobilized the aneurysm to the origin of the hepatic artery on the aorta which was normal in caliber. The aneurysm also involved the GDA. There was normal artery at the hepatic proper. After harvesting saphenous vein we placed an interposition bypass from the proximal hepatic artery to hepatic proper and removed the aneurysm. We attempted to mobilize the GDA and sew it in a side fashion with the hepatic proper but the vessel tore. Instead we bypassed from the origin of the hepatic artery to the hepatic proper. After our bypass the liver appeared viable. On exploration, the hepatic proper divided into the left/right hepatic arteries. There was good back-bleeding of the GDA due to collateral circulation of the SMA, thus we ligated the GDA. Post-op he recovered well with with normal liver function and went home. This case proved to be challenging based on understanding hepatic anatomy and the many anomalies that can be encountered.

Back to 2019 Abstracts
