Percutaneous Retrograde Left External Carotid Artery Coil Embolization for Management of Hemorrhage from a Persistent Proatlantal Intersegmental Artery
Hunter M. Ray, MD1, Joshua D. Kuban, MD2, Alda L. Tam, MD2, Tam T. Huynh, MD2, George T. Pisimisis, MD2.
1The University of Texas Health Science Center at Houston (UT Health), McGovern Medical School, Houston, TX, USA, 2The University of Texas MD Anderson Cancer Center, Houston, TX, USA.
DEMOGRAPHICS:
64-year-old male with T2N2b squamous cell carcinoma (SCC) of the left tonsil.
HISTORY:
The patient underwent neoadjuvant chemoradiation, but developed persistent disease at follow-up. Re-operative resection involved trans-oral robotic surgery with partial left pharyngectomy and glossectomy with left neck dissection (levels 2-4) necessitating ligation of the external carotid artery (ECA) origin. He presented with acute oropharyngeal bleeding one month after surgery.
PLAN:
Due to sudden onset of large volume hemorrhage digital pressure was applied trans-orally, followed by emergent awake tracheostomy for airway protection/control. Direct laryngoscopy revealed necrotic left stylohyoid ligament with surrounding soft tissue necrosis and profuse arterial bleeding, which was packed for hemostasis. The patient was then transferred to a hybrid operating room with fluoroscopy (Zeego,Siemens) and CT scan (Definition Edge,Siemens) capabilities for further evaluation and treatment.
DISCUSSION:
Carotid artery bleeding was suspected. Cerebral angiography revealed complete occlusion of the left common (CCA) and internal carotid arteries (ICA) without contrast opacifcation of the left distal ICA or ECA. Right ICA catheterization, demonstrated brisk cross filling of the left anterior and middle cerebral arteries without visible bleeding source. Selective left vertebral (dominant) angiogram demonstrated a persistent proatlantal intersegmental artery (Fig 1A,white arrow) arising from the distal left vertebral artery and retrograde perfusing the left ECA, terminating as an irregular stump with vasospasm (Fig 1A,black arrow). Intraoperative computed tomography angiography demonstrated an arterial blush at the previous surgical site from ECA branches (Fig 1B,circle). Coil embolization of the left CCA was performed to prevent potential recanalization and embolic stroke. Without the protection of therapeutic anticoagulation and acknowledging the left carotid occlusion and vertebral dominance, we considered the option of retrograde ECA embolization with microcatheter through the proatlantal branch as more time demanding and higher risk for left vertebral complications. Therefore, the left ECA was accessed percutaneously under duplex guidance through the parotid gland and via microcatheter a retrograde coil embolization of the irregular ECA stump and 2 cm trunk was performed, to include the suspicious branches (Fig1C,black arrow). All packings were removed without active bleeding and the patient awoke neurologically intact and remained without recurrent bleeding at one year follow-up. 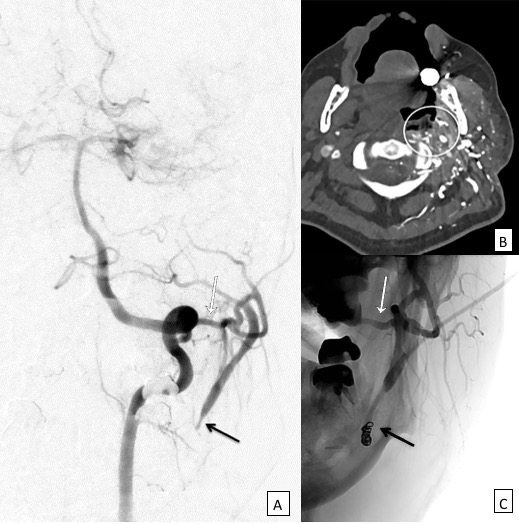
Back to 2019 Abstracts
