Physician-modified four-vessel fenestrated stent graft to treat ruptured juxtarenal abdominal aortic aneurysm in a patient with previous abdominal aortic repair
Tiziano Tallarita, MD, Mendes Bernardo, MD, Thomas Bower, MD, Gustavo Oderich, MD.
Mayo Clinic, Rochester, MN, USA.
DEMOGRAPHICS: 73-year-old male with previous open repair of an inflammatory juxtarenal abdominal aortic aneurysm (AAA) with an aorto-aortic tube graft and chronic left common and external iliac artery occlusion with chief complaint of abdominal pain.
HISTORY: Patient presented with acute onset abdominal pain and hypotension in a community hospital emergency department. Computed tomography angiography (CTA) demonstrated ruptured para-anastomotic AAA adjacent to the renal arteries (Figure). During emergent air transportation, patient received multiple units of RBC, FFP and Kcentra for INR of 4.5. On presentation in our institution, patient was diaphoretic, interactive, with systolic blood pressure of 95mmHg, palpable right femoral and upper extremities pulses. Hemoglobin was 10.3mg/dL, creatinine 1.6mg/dL, and INR 1.3. Previous medical history included morbid obesity (BMI 45), hypertension, hyperlipidemia, type 2 diabetes mellitus, coronary artery disease, atrial fibrillation on warfarin, obstructive sleep apnea, chronic obstructive pulmonary disease and prior smoking.
PLAN: Given the high risk for redo open repair and the improved hemodynamics after initial resuscitation, endovascular treatment with a 4-vessel fenestrated physician-modified stent graft (PMEG) with preloaded wires was performed. The stent graft was planned using centerline of flow image reconstruction (Figure). Onlay fusion CTA was utilized to facilitate identification of target vessels. A 36x32x209mm Cook Zenith Alpha™ stent graft was modified expeditiously and delivered through percutaneous right femoral access, while the fenestrations were cannulated from the right brachial approach using four preloaded wires. A 36x12x82mm Zenith aorto-iliac converter™ and 16x20x56mm iliac extension were subsequently deployed to exclude the aneurysm sac (Figure). Cone beam CT (CBCT) scan was performed and demonstrated no attachment endoleaks and patent target vessels. Patient recovered uneventfully and was discharged on post-operative day 9.
DISCUSSION: Physician-modified stent grafts are an important tool for urgent repair of complex AAA in patients not fit for open surgery. This case illustrates successful use of a PMEG in a patient with a true aortic rupture not otherwise suitable for a redo open repair. In the emergent setting, adjunctive tools such as preloaded wires, onlay fusion and CBCT scan can facilitate vessel cannulation, decrease radiation exposure and expedite operative time, potentially improving perioperative outcomes. 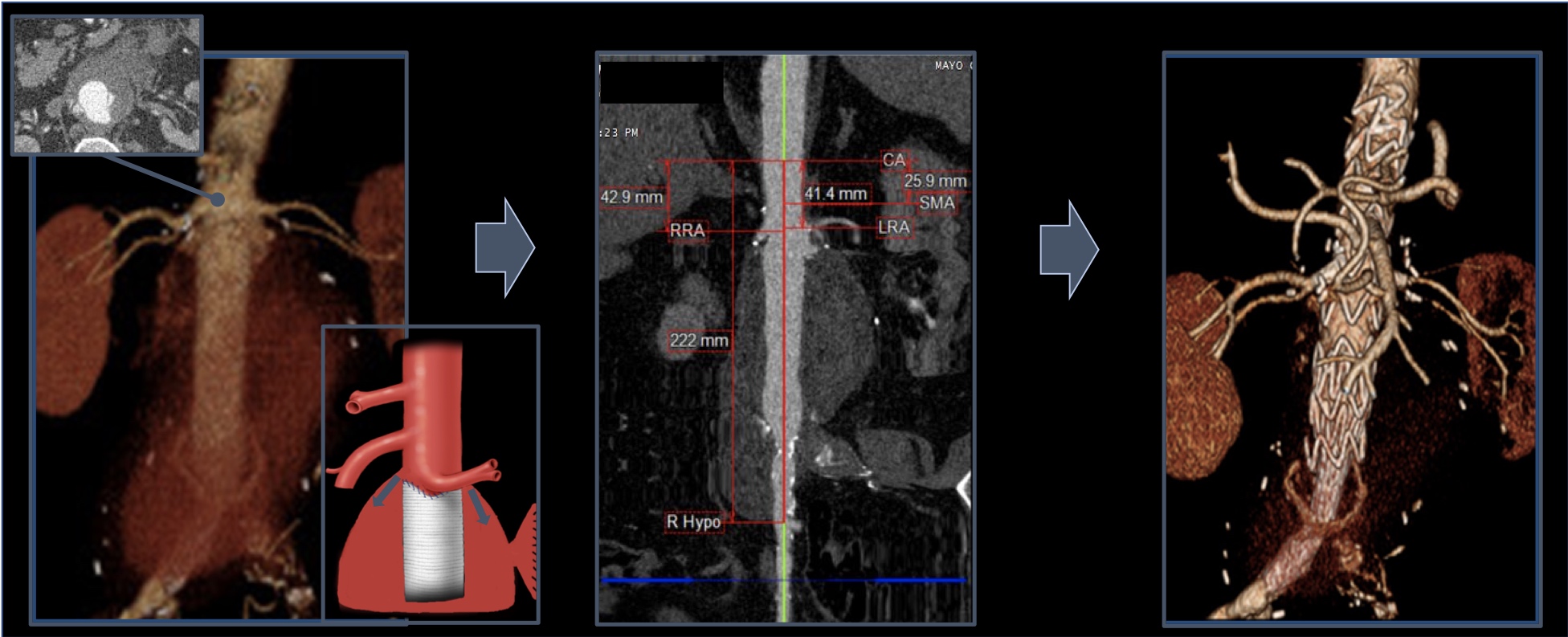
Back to 2019 Abstracts
