Endovascular Treatment for Symptomatic Aortic Thrombus
Apurva Trivedi, David Mariner, MD, Melissa Obmann, DO, Boyong Song, MD.
Geisinger Wyoming Valley, Wilkes-Barre, PA, USA.
OBJECTIVES
Thoracic aorta mural thrombus is underdiagnosed and usually only reported after embolic events. Current treatment options include medical management with anticoagulation, open and endovascular surgical therapies. We present a case series of three young women with symptomatic descending thoracic aortic thrombus of which two were treated with stent grafts.
METHODS
Patient A is a 45-year old female with history of cervical cancer presented with abdominal pain. A computed tomography angiography (CTA) showed splenic infarction with a large partially occlusive thrombus in the descending aorta. An MRI excluded primary aorta tumor. Anticoagulation was initiated and she was taken to the operating room the following day with successful thoracic aortic stent graft (Medtronic Valiant, Minneapolis, MN) placement to trap the thrombus.
Patient B is a 36-year old female with history of right lower extremity bypass two years ago from an embolic event secondary to thoracic aortic thrombus. She was anticoagulated with subsequent complete resolution of the thrombus. Recently, she presented with acute left leg ischemia and was found to have recurrent thrombus in the thoracic aorta. She underwent thromboembolectomy of her left leg and subsequently underwent coverage of the thrombus with stent graft (Medtronic Valiant, Minneapolis, MN).
Patient C is a 51-year old female with history of atrial fibrillation and DVT presented with acute abdomen and found to have a superior mesenteric artery embolus with large non-occlusive thrombus from proximal-mid descending thoracic aorta. She underwent emergent SMA embolectomy and was placed on anticoagulation.
RESULTS
Patients A and B were discharged on anticoagulation. Follow up CTAs displayed stent grafts without additional thrombus burden.
For Patient C, a repeat CTA revealed the thrombus migration to the perivisceral aorta. Open aortic thromboembolectomy via retroperitoneal approach was contemplated. However, she arrested and expired secondary to a large retroperitoneal hematoma.
CONCLUSIONS
Although not without risk, aggressive treatment of primary symptomatic aortic thrombus with anticoagulation and endovascular stent graft exclusion can be effective and potentially life-saving therapy. Larger series of patients are needed to further delineate short and long-term outcomes. 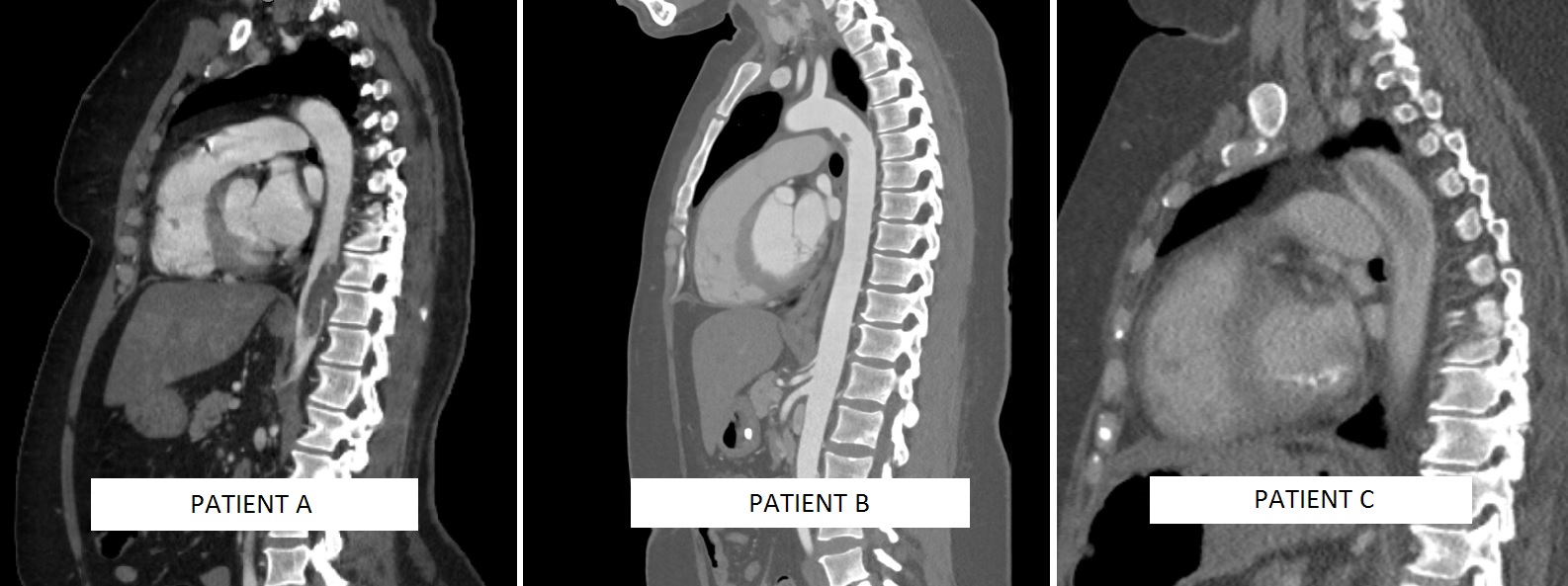
Back to 2019 Abstracts
