Machine Learning-Based Prediction of Abdominal Aortic Aneurysms for Individualized Patient Care
Kelli L. Summers, MD1, Edmund K. Kerut, MD1, Filip To, PhD2, Claudie M. Sheahan, MD1, Malachi G. Sheahan, III, MD1.
1Louisiana State University, New Orleans, LA, USA, 2Mississippi State University, Starkville, MS, USA.
OBJECTIVES: Machine learning (ML) can process complex nonlinear relationships between predictors. ML has had superior outcome predictions in a variety of settings including Emergency Department triage and pediatric traumatic brain injury. Our goal was to examine the utility of ML models for predicting risk of abdominal aortic aneurysm (AAA).
METHODS: A machine learning model to predict the presence of AAA (>3cm) was created from the database of a national non-profit screening organization (AAAneurysm Outreach). Participants self-reported demographics and co-morbidities. The model is a two-layered feed-forward shallow network. Sensitivity analysis for each input parameter was performed to identify which parameters had the most influence on the algorithm. The ML model then generated AAA probability based on patient characteristics.
RESULTS: A 10,329 patient cohort with a AAA prevalence of 2.70% was analyzed. Consistent with logistic regression analysis, the ML model identified the following predictors of AAA: Caucasian ethnicity, male gender, increasing age, and recent or past smoker with recent smoker having a more profound affect (P < .05). Sensitivity analysis demonstrated the most important parameters to the model were hypertension, smoking, and family history of AAA. Interestingly, the ML model showed BMI was associated with likelihood of AAA. Re-evaluating the data, this was seen for Caucasian male non-smokers age 50-65 with a BMI >25 (P < 0.5), as well as in smokers. The opposite was true for older, Caucasian, non-obese male smokers - there was an increased prevalence of AAA in comparison to overweight smokers (P < .01). These relationships together with the ML model for a BMI of 25 are shown in Figure 1. This reverse effect of BMI on AAA prevalence with older compared to middle-age was also seen in females and male never smokers.
CONCLUSIONS: We have successfully developed a machine learning model based on a AAA screening database. This has unveiled a complex relationship of AAA prevalence with BMI. Furthermore, this ML model has the potential to be transitioned to a clinical setting to deliver more precise screening recommendations. 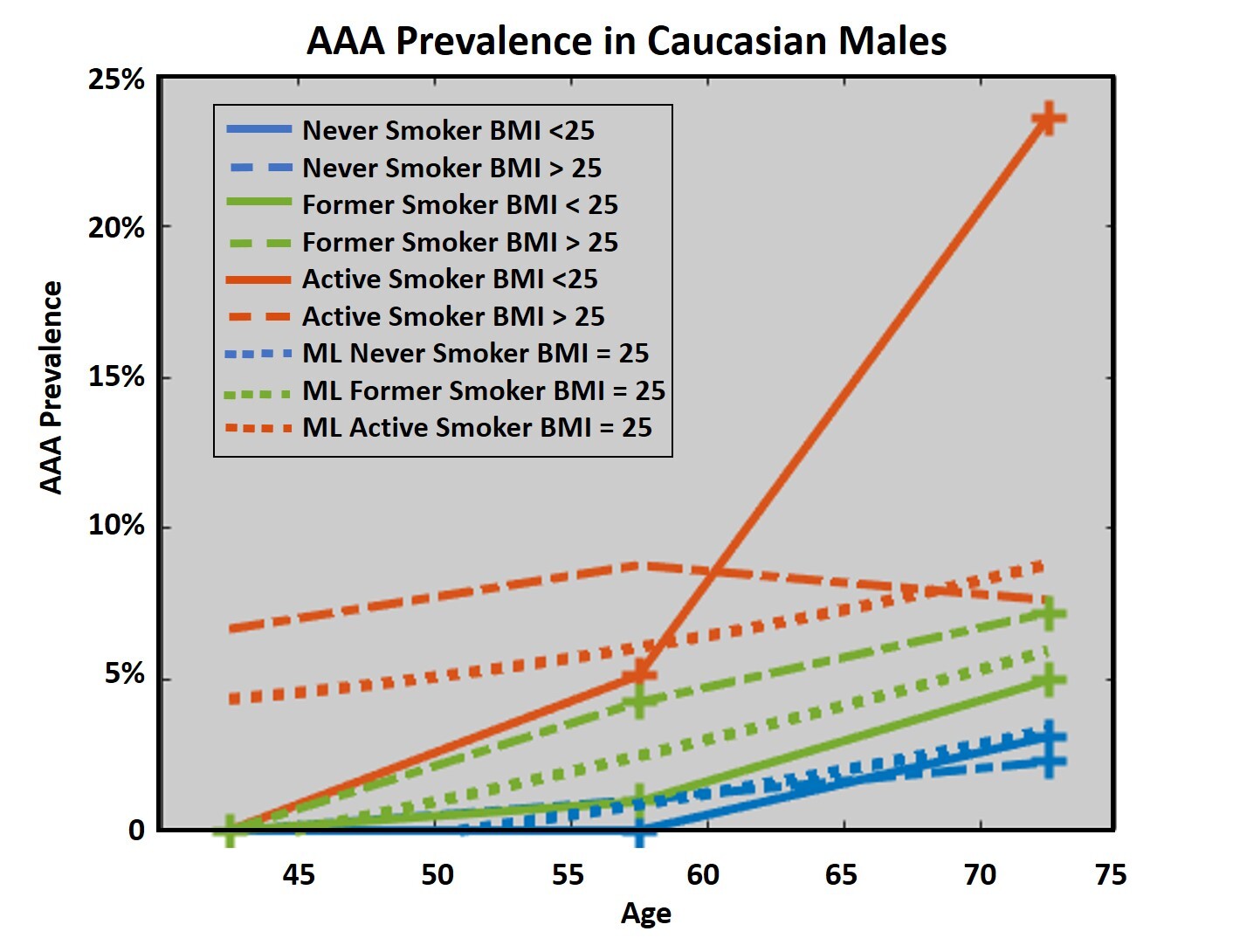
Back to 2020 Abstracts
