Early And Late Results Of Reconstruction With Renal And Visceral Bypasses During Open Thoracoabdominal Aortic Aneurysm Repair
Parvathi W. Balachandran, MD PhD, Manju Kalra, MD, Alberto Pochettino, MD, Kevin L. Greason, MD, Edward D. Gifford, MD, Jill K. Colglazier, MD, Gustavo S. Oderich, MD, Randall R. DeMartino, MD, Thomas C. Bower, MD.
Mayo Clinic, Rochester, MN, USA.
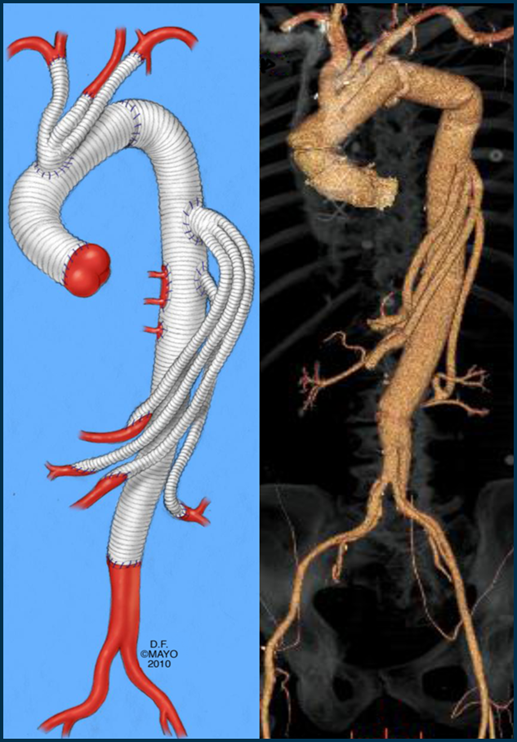
Objective: Open Thoracoabdominal aortic aneurysm (TAAA) repair remains an important treatment option for medically fit patients and those with connective tissue disease. In an effort to prevent delayed patch aneurysm of visceral segments we perform reconstruction using individual long bypass grafts to visceral and renal vessels, arising proximal to the site of intercostal patches (Figure). The aim of this study was to evaluate immediate and long-term outcomes of this strategy for open TAAA repair and specifically of the visceral/renal bypasses (VRBs). Methods: Data from consecutive patients undergoing open TAAA repair with VRBs between 2002 and 2018 were retrospectively reviewed. Demographic and anatomic data, operative details, mortality, morbidity and long-term follow-up specifically evaluating visceral / renal branch vessel patency were analyzed. Results: There were 122 patients, 84 male, 38 female with median age 58 years (IQR 44-69); with 4 Type I, 88 Type II, 17 Type III and 13 Type IV TAAAs. Connective tissue disorder was identified in 30% patients and dissection in 57%. Mean SVS/AAVS comorbidity score was 7.9 (95% CI 6.4-9.0). Repairs were elective in 91% patients; deep hypothermic circulatory arrest (DHCA) was employed in 90% Type I-III and no Type IV TAAAs. Spinal drainage was performed in 37%. All repairs included VRBs; median number of intercostal artery pairs re-implanted was 3. Overall 30-day mortality was 15%. Morbidity among patients repaired with and without DHCA respectively was paraplegia (3% vs 13%), stroke (5% vs 9%), myocardial infarction (1% vs 15%), and renal failure requiring hemodialysis (11% vs 39%, 2% permanent). Median clinical follow-up was 44 months (range 11-188). Median imaging follow-up, available in 107 patients, was 40 months (range 12-148). Overall VRB graft patency at follow-up was 96%; celiac 98%, SMA 98%, renal 95%, accessory renal 75% (3/4). Patency of intercostal patches was 93% with aneurysmal degeneration in 2 patches; one successfully treated with endograft repair at 3 years. Conclusions: TAAA repair with debranching of visceral and renal vessels with long bypasses can be safely performed under DHCA, with acceptable early mortality and morbidity. Long-term patency of these bypasses is excellent with the advantage of avoidance of patch aneurysms.
Back to 2020 Abstracts
