The Association Between Intraoperative Hypotension And Postoperative Adverse Outcomes After Vascular Surgery
Livia de Guerre, MD, Valluvan Rangasamy, Xinling Xu, Marc Schermerhorn, Victor Novack, Balachundhar Subramaniam.
Beth Israel Deaconess Medical Center, Boston, MA, USA.
OBJECTIVES: Intraoperative hypotension (IOH) is associated with adverse outcomes. However, there is no universally accepted definition for IOH. Vascular surgical patients are unique due to their underlying disease and increased baseline systolic and pulse pressures. It is unknown whether these patients need a different threshold to define IOH. Also, it is unclear if preoperative blood pressure (BP) or surgical approach could influence the associations between IOH and adverse outcomes. Therefore, we explored the relationship between varying thresholds of IOH and adverse postoperative outcomes, and the interaction with both preoperative blood pressures and surgical approach (open vs endovascular).
METHODS: In this retrospective, observational study using a prospectively collected institutional vascular surgical database, we included patients undergoing vascular surgery (open and endovascular abdominal aneurysm repair, lower extremity amputation and, suprainguinal and infrainguinal bypass) from 2011 to 2018. IOH was defined using an absolute threshold of MAP < 65mmHg or a relative threshold of MAP > 20% decrease from baseline and was characterized as total duration below the threshold, Area Under the Curve (AUC), and Time Weighted Average (TWA). The primary outcome was a predefined composite of postoperative in-hospital complications including mortality, stroke, myocardial infarction, congestive heart failure, and acute kidney injury.
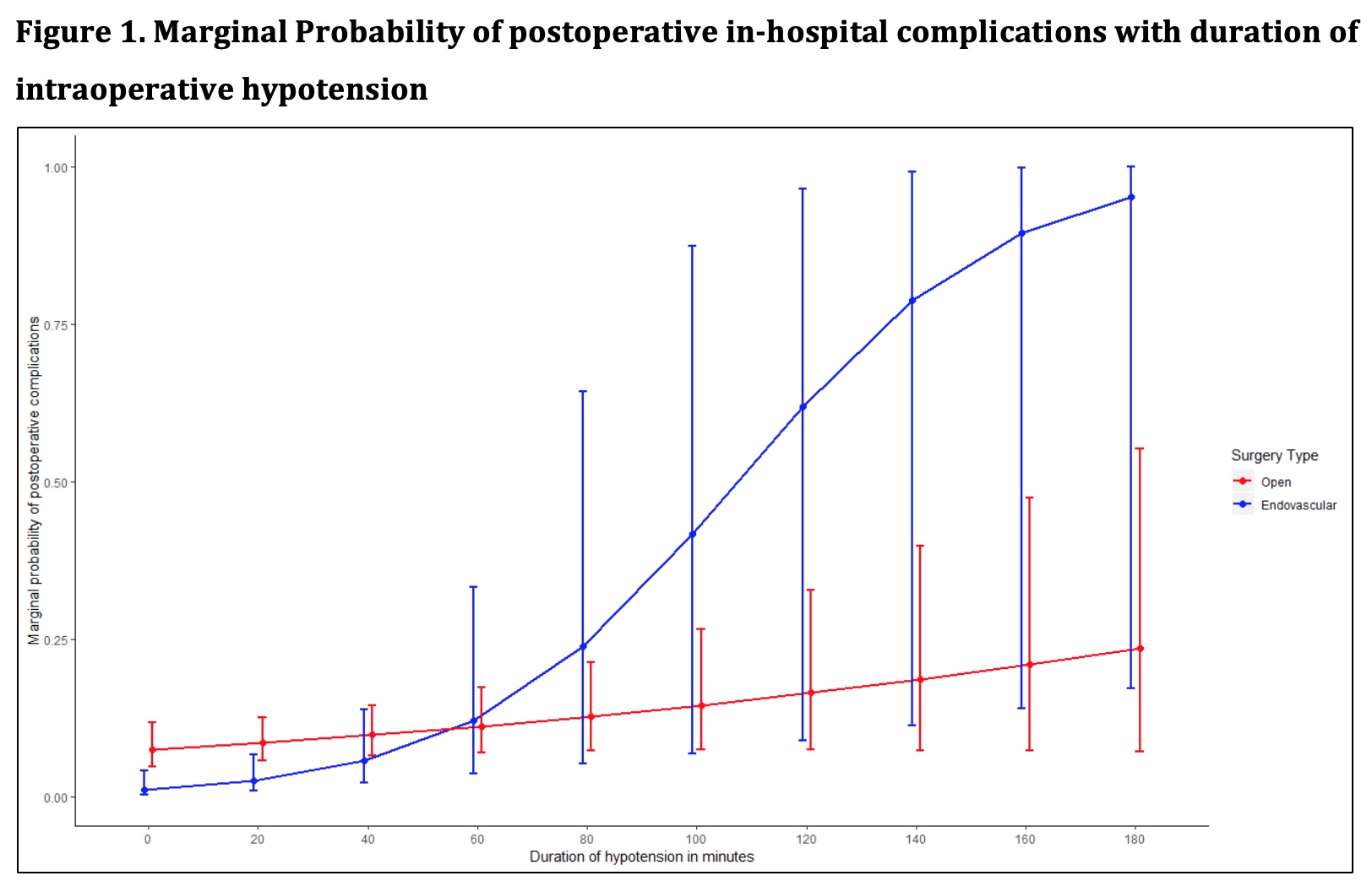
RESULTS: Of the 566 patients included, 46 (8.1%) had an in-hospital complication. Duration of MAP < 65mmHg in minutes (OR 1.01, 95%CI 1.00 - 1.02, P = 0.004) was significantly associated with in-hospital complications. No associations were seen with duration of MAP >20% decrease from baseline (Table 1). The association of IOH was stronger for EVAR procedures than open procedure (interaction P=.031, Figure 1). No interactions were seen with preoperative pulse pressure or systolic hypertension.
CONCLUSIONS: In vascular surgical patients, absolute but not relative BP thresholds were significantly associated with worse outcomes. Targeted prevention of IOH in patients undergoing vascular surgery might result in a reduction of adverse outcomes. 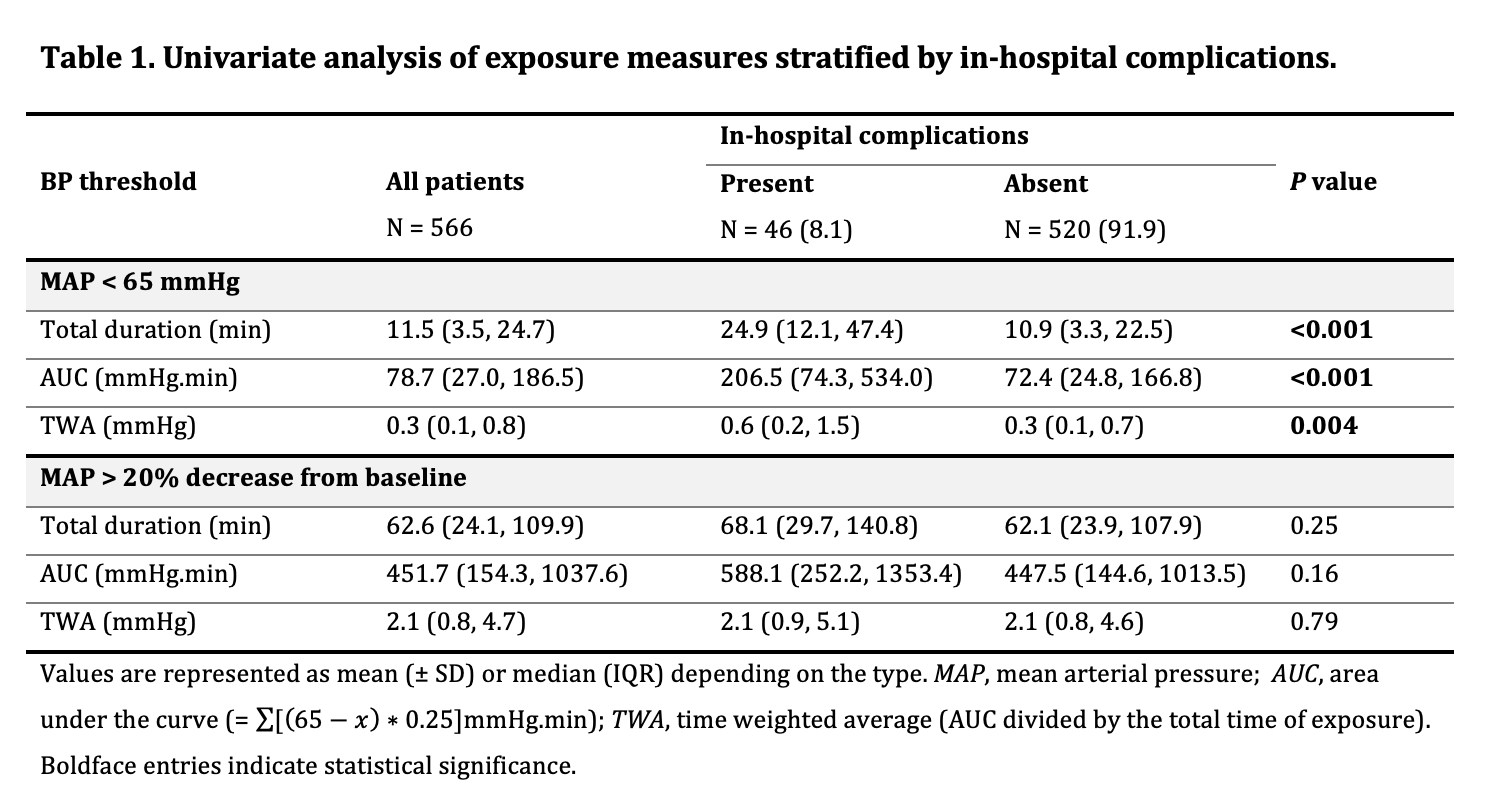
Back to 2020 Abstracts
