Case Volume Variation Between Traditional Vs. Integrated Vascular Surgery Training Programs
Susanna WL de Geus, MD PhD, Alaina D. Geary, MD, Stephanie Talutis, MD MPH, Teviah E. Sachs, MD MPH, Jennifer F. Tseng, MD MPH, Jeffrey J. Siracuse, MD.
Boston Medical Center, Boston, MA, USA.
OBJECTIVES: The present study compares the operative experience of graduates from traditional vascular surgery (5 + 2) and integrated vascular surgery training programs (0 + 5) using contemporary operative case log data.
METHODS: The Accreditation Council for Graduate Medical Education (ACGME) integrated vascular surgery, vascular surgery fellowship, and general surgery case logs for trainees graduating between 2013 and 2018 were queried for vascular surgery procedures. ‘Senior’ cases were categorized as cases logged as ‘Surgeon Fellow’ by 5 + 2 trainees or ‘Surgeon Chief’ (PGY-4,5) by 0 + 5 trainees. Overall case volume was defined as the combined volume of cases logged as ‘Surgeon Junior’, ‘Surgeon Chief’, ‘Surgeon Fellow’, ‘Teach Assist’, ‘First Assist’, or ‘Secondary procedure’. To reflect total vascular experience, all vascular cases done during general surgery residency were combined with cases performed during vascular surgery fellowship. Mean case volumes were compared for all operations/procedures.
RESULTS: Over the study period, 5 + 2 trainees logged significantly more mean ‘Senior’ carotid endarterectomies (47 vs. 29; p<0.001), carotid artery stents (10 vs. 5; p=0.001), open thoracic aorta (1 vs. 0; p=0.004), endovascular thoracic aorta (15 vs. 8; p<0.001), and endovascular abdominal aortic repairs (45 vs. 28; p<0.001), open mesenteric (4 vs. 2; p<0.001), and femoral-popliteal/tibial (vein) (10 vs. 6; p=0.002) bypasses compared to 0 + 5 trainees. Both groups performed similar mean numbers of open aortic aneurysm repairs (6 vs. 4; p=0.070), thoracoabdominal aortic aneurysms repairs (4 vs. 2; p=0.149), and femoral-popliteal prosthetic (13 vs. 5; p=0.212) bypasses. The overall case volume of open mesenteric bypasses (mean, 5 vs. 4; p<0.001) was higher for 5 + 2 trainees, whereas the overall case volume endovascular abdominal aorta aneurysm repairs (mean, 62 vs. 69; p=0.051) was higher for 0 + 5 trainees. For all other procedures, the overall case volume was comparable for 5 + 2 and 0 + 5 trainees.
CONCLUSIONS: Although both pathways graduate trainees with a similar overall surgical experience, 5 + 2 trainees log significantly more ‘Senior’ cases. Further studies investigating potential variation in operative autonomy between both pathways are necessary. 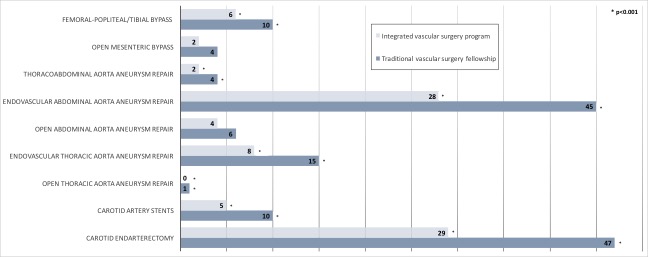
Back to 2020 Abstracts
