Variations In The Medical Managements Of Iliocaval Deep Vein Thrombosis: Time For A Consensus.
Ashlei C. Beiswenger, MS, BSE, Jones P. Thomas, MD, Michael P. Brown, DO, Norman H. Kumins, MD, Vikram S. Kashyap, MD, FACS, Vivek R. Sreeram, MD, Karem C. Harth, MD, MHS.
University Hospitals Cleveland Medical Center, Cleveland Heights, OH, USA.
Objective:
Medical management of deep vein thrombosis (DVT) in the iliocaval system requiring intervention lacks consensus. Duration of therapy and type of therapy has not undergone rigorous evaluation. In the setting of lytic therapy and stent placement for compressive or chronic lesions, duration and type of anticoagulation in addition to the role of antiplatelet agents is unclear. The purpose of this study was to evaluate practice patterns in anticoagulation and antiplatelet therapy regimens among various groups treating DVT in the iliocaval system.
Methods:
This study was a single-institution, retrospective review of all patients who received interventional treatment for iliocaval DVT over a 2 year period (2017-2018). Information on subjects’ demographics, characteristics of the DVTs, medication on presentation for treatment, characteristics of treatment, and post-procedural medical management were collected. Data were stratified by specialty. Single-variate analyses comparing continuous variables used t-test, and those comparing categorical variables used the 𝜒;;;2 test.
Results:
A total of 49 interventions were identified, as detailed in Table 1. Among these specialties, there was a statistically significant difference in intravascular ultrasound usage (VS: 79.3%, IC: 33.3%, IR: 42.9%; p=0.02), number of stents placed (VS: mean (standard deviation) 2(1), IC: 0(0), IC: 1(1), p<0.01), stent placement in the common iliac veins (VS: 79.3%, IC: 0.0%, IR: 64.3%; p<0.01), and stent placement in the external iliac veins (VS: 69.0%, IC: 0.0%, IR: 35.7%; p<0.01). For medical management after intervention, IR prescribed direct oral anticoagulants (DOACs) at a significantly higher rate than other specialties (78.6%, 34.5%, 33.3%, respectively; p=0.02), and VS and IC prescribed warfarin significantly more often (58.6%, 66.7%, 21.4%, respectively; p=0.05). Duration of anticoagulation therapy did not vary significantly among specialties. IR also prescribed aspirin after intervention more often than VS or IR (64.3%, 17.2%, 33.3%, respectively; p<0.01) and was the only group to prescribe dual antiplatelet therapy in addition to anticoagulation.
Conclusion:
This data demonstrates that there is significant variation across specialties in approaches to the medical management to treating DVTs despite similar cohort of patients. Further studies are needed to achieve consensus regarding optimal management of these complex group of patients. 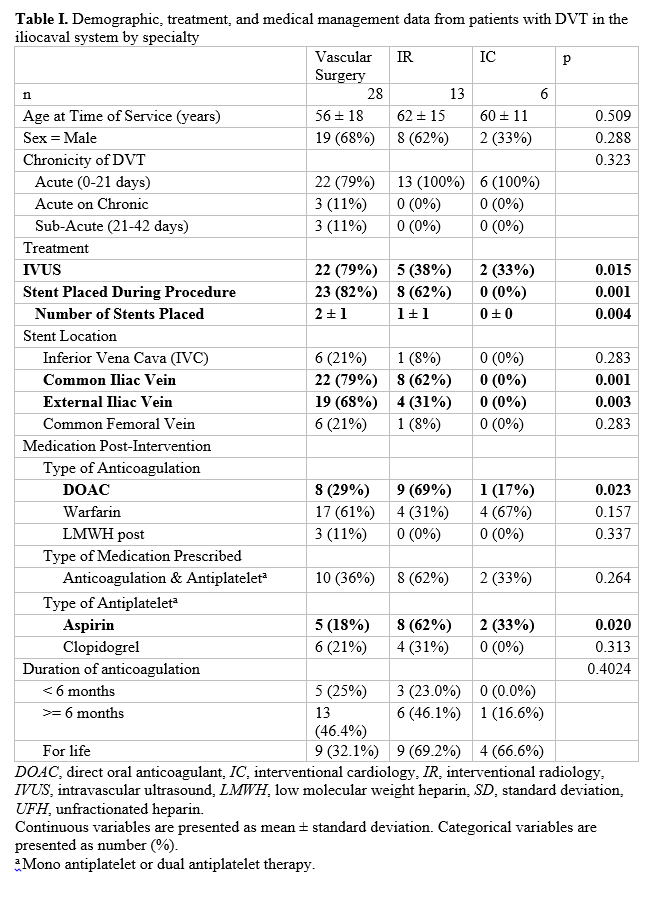
Back to 2020 Abstracts
