Impact Of National Adoption Of Endovascular Revascularization On A Regional Referral Center Specializing In Management Of Chronic Mesenteric Ischemia
Tabassum A. Khan, MD, MPH, Jeffrey D. Crawford, MD, Salvatore T. Scali, MD, Kristina A. Giles, MD, Martin R. Back, MD, Thomas S. Huber, MD, PhD, Gilbert R. Upchurch, Jr., MD, Dean J. Arnaoutakis, MD, MBA.
University of Florida, Gainesville, FL, USA.
Objective: Nationally, endovascular revascularization(ER) is more common than open mesenteric bypass(OMB) for management of chronic mesenteric ischemia(CMI), but the overall incidence of OMB has remained stable. Importantly, patients ineligible for ER due to anatomic factors frequently undergo OMB but fewer institutions contemporaneously offer these therapies due to operative complexity and resource utilization. Notably, the impact of increasing ER adoption on referral hospitals specializing in CMI management remains poorly defined. This analysis sought to determine the temporal variation in ER/OMB utilization and outcomes within a large, regional referral center specializing in CMI management.
Methods: A retrospective analysis of a single academic institution’s prospectively collected database was performed to identify all CMI patients(2002-2018). The primary end-point was temporal change in revascularization strategy(eras: 2002-2007, 2008-2013, 2014-2018). Secondary end-points included evolution in complications, re-intervention, and survival.
Results: 189 patients(OMB[n=109;antegrade-91%,retrograde-8%], ER[n=80; stent-91%,angioplasty-9%]) were identified. OMB became significantly more common in the most recent era(84%-OMB;p<.0001). OMB patients were significantly younger(66±11 vs. ER,71 ±11years;p=.006) and more likely to have undergone prior ER(OMB-36% vs. ER-17%;p=.005). Crude rate of any major complication was greater with OMB(OMB-54% vs. ER-20%;p<.0001) but 30-day mortality was similar(OMB-6%[n=6] vs. ER-1%[n=1];p=.012). However, there was greater frequency of restenosis and/or recurrent symptoms after ER(50% vs. OMB-9%;p<.0001). Five-year freedom from re-intervention and/or re-stenosis was significantly higher for OMB(77±7 % vs. ER-33±6%;log-rank p< 0.0001). There was a non-significant trend towards improved five-year survival after OMB(70±5% vs. ER-60±6%;Cox model p=.06). With risk-adjustment, no significant difference was detected regarding complications(OMB:p=0.34; ER:p=0.35) or 30-day mortality risk(OMB: p=0.11; ER:p=0.20) when comparing outcomes across all three eras(Figure). OMB previously had higher risk of post-operative complications vs. ER[2002-2007(p<0.001); 2008-2013(p=0.021)], but from 2014-2018, no difference was observed(p=0.235).
Conclusions: Significantly increased OMB utilization occurred over time predominantly due to an increasing proportion of ER failures and/or poor anatomic suitability, highlighting how CMI referral centers may not reflect national trends. Despite the known morbidity of OMB, in appropriately selected patients, both therapies can provide comparable outcomes when managed at a high-volume referral center. This information has important implications on surveillance strategies and a need to designate centers of excellence that can offer OMB for late ER failures. 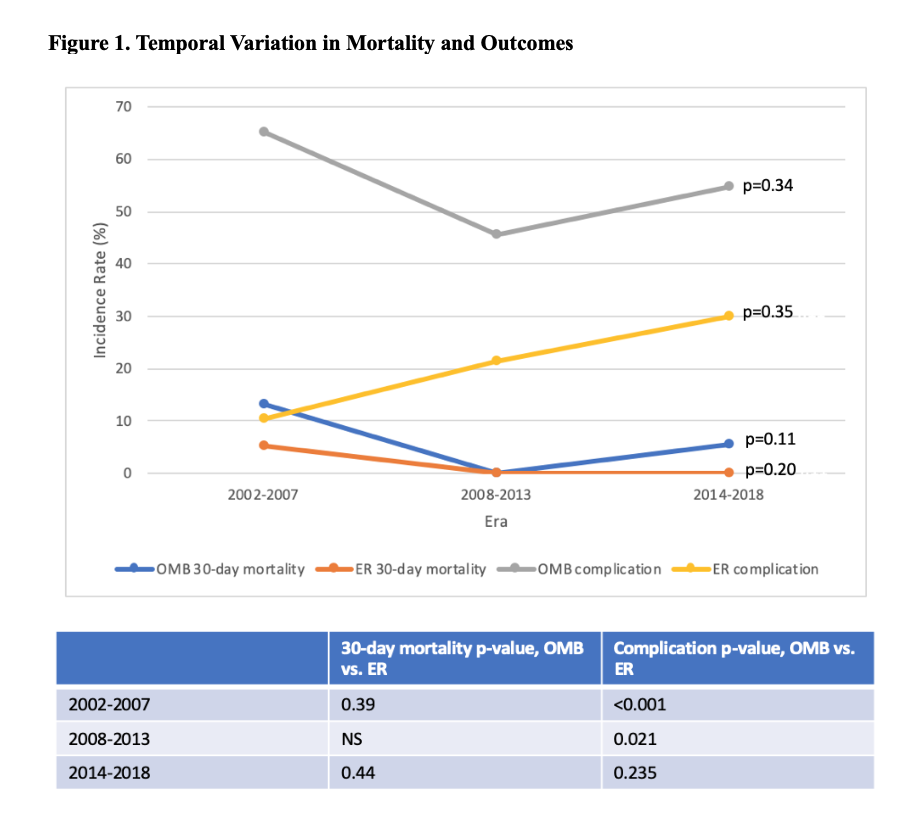
Back to 2020 Abstracts
