Neutrophil-to-Lymphocyte Ratio Associated With Rates Of Adverse Events After Endovascular Aneurysm Repair (EVAR)
David Octeau, Christopher Faries, Hanna Barnes, Kenneth R. Nakazawa, MD, Windsor Ting, MD, Michael L. Marin, MD, Peter L. Faries, MD, Rami O. Tadros, MD.
Icahn School of Medicine at Mount Sinai, New York, NY, USA.
OBJECTIVES: The blood neutrophil-to-lymphocyte ratio (NLR) is a surrogate biomarker of systemic inflammation with important prognostic significance in multiple disease processes, including cardiovascular diseases. It is inexpensive, widely available, and may be related to the outcomes of patients after surgery. We aimed to investigate the possible association of NLR with the outcomes of patients following endovascular aneurysm repair (EVAR).
METHODS: This single-center, retrospective study of a prospectively maintained database evaluated 734 patients with a diagnosed abdominal aortic aneurysm (AAA) who underwent EVAR and were longitudinally followed between 2001 and 2018. NLR was defined as the ratio of absolute neutrophil count to absolute lymphocyte count. The event-free interval (EFI) was used to evaluate outcomes using the appropriate univariate and multivariate survival models. Adverse events included endoleaks requiring reintervention, graft infections, and vascular events requiring surgical reintervention, such as bowel, spinal or limb ischemia. The effect of clinical variables on NLR was further investigated.
RESULTS: The median NLR for all patients was 3 [2.2 - 4.6]. The NLR levels were significantly associated with EFI in a univariate analysis (Table 1; HR 1.05 [1.01 - 1.08]; p = 0.039). A cut-off point of 3.9, selected based on the maximally selected log-rank statistic, was determined to provide the most separation between the EFI of the high and low NLR groups. Multivariate analysis revealed that NLR (Table 1; HR 1.031 [1.01 - 1.05]; p = 0.004) remained an important predictor of outcomes in a multivariate analysis controlling for characteristics such as comorbidities, age, and maximal aortic diameter. No measured clinical variables were found to significantly affect patient NLR.
CONCLUSIONS: NLR was significantly associated with adverse events post-EVAR. It remains unclear whether NLR is directly linked to adverse events post-EVAR or whether it is a surrogate for an inflammatory state which predisposes patients to higher risk of adverse events. 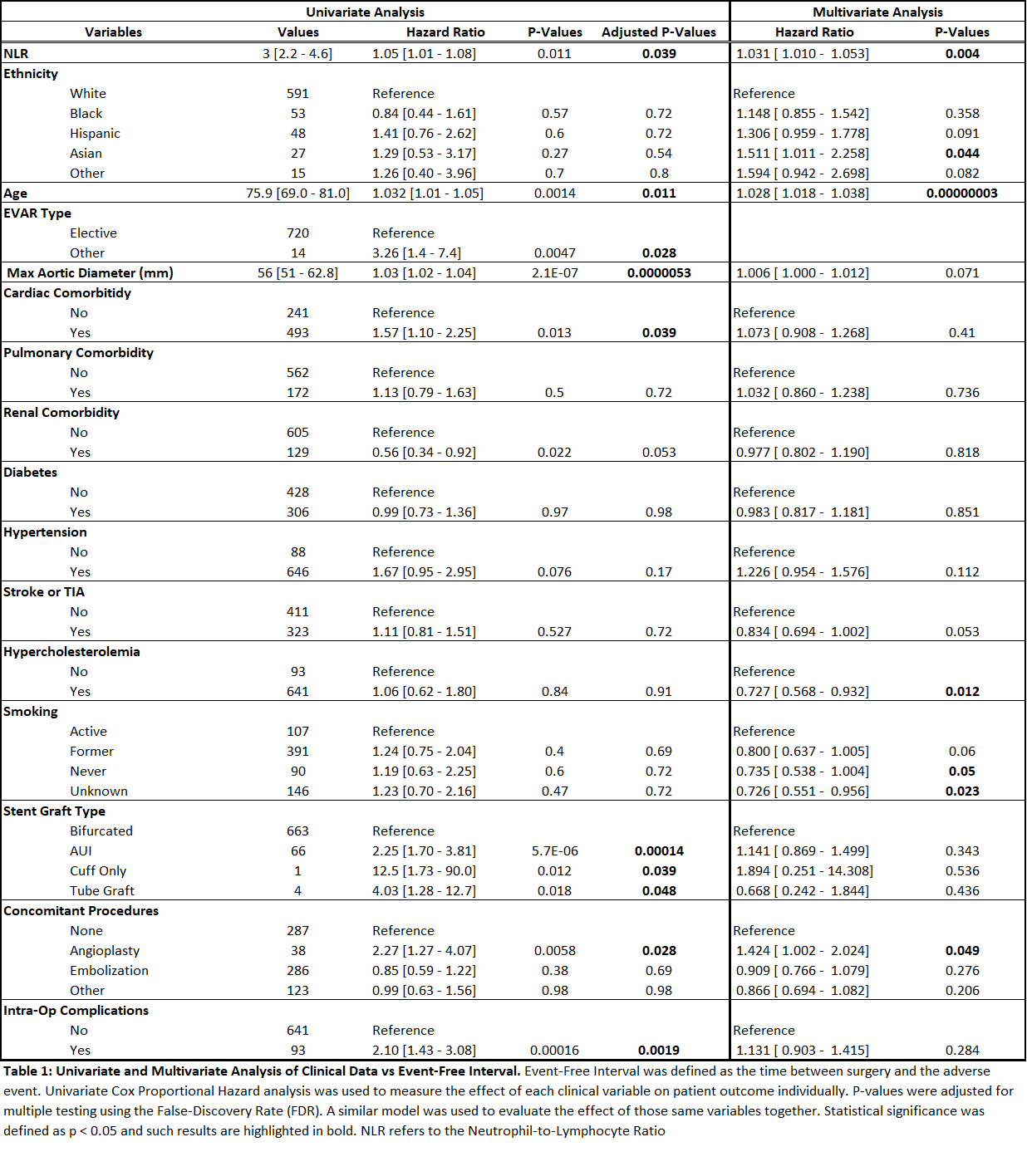
Back to 2020 Abstracts
