Transcarotid Artery Revascularization (tcar) In The Emergency Setting
Josh Gutierrez, MD, Georgios Tzavellas, MD, Angela Kokkosis, MD.
Stony Brook University Hospital, Stony Brook, NY, USA.
Transcarotid artery revascularization (TCAR) in the emergency setting
Demographics: The patient is a 78-year-old male with history of hypertension, hyperlipidemia, PFO, and a recent left frontoparietal infarct.
History: The patient had a left cerebrovascular accident (CVA) with expressive aphasia and right sided weakness for which workup revealed complete occlusion of the left common and internal carotid arteries, 90% stenosis of the right internal carotid artery, and an occluded right vertebral artery. The patient was placed on dual antiplatelet therapy and a statin. At one week follow-up, he had almost completely recovered from the CVA except for lingering anomic aphasia. He was scheduled 6 weeks from his CVA for a right carotid endarterectomy (CEA) for future stoke prevention. Four days prior to his scheduled CEA, the patient presented in the emergency department with severe reoccurring expressive aphasia.
Plan: The patient underwent a brain CT perfusion study. This revealed a perfusion deficit involving a large area of the left frontal and parietal lobes secondary to the delayed perfusion from collateral flow from the right hemisphere. The neurology team diagnosed this clinical picture as stroke-in-evolution with a large ischemic penumbra, and high risk for progression to complete hemispheric stroke. Therefore, we decided to proceed with an emergent right carotid revascularization. We performed a transcarotid artery revascularization(TCAR) in order to avoid any clamp time of internal carotid artery; and to perform the intervention under local anesthetic only, to enable us to monitor his neurologic status. Intraoperatively, the stenting of the carotid artery was technically challenging given the heavy calcification. This resulted in a flow reversal time of 123 minutes. However, the patient remained neurologically and hemodynamically stable. After 3 days of monitoring by the neurology service, he was discharged without complications. At 6-month follow-up, the patient had significant neurologic improvement, and duplex demonstrated a patent carotid stent.
Discussion: Emergent carotid revascularization is rarely performed and TCAR may represent a comparable alternative to CEA in this setting. Additionally, while the collateral pathways to the intracranial circulation are poorly understood, flow reversal appears to be safe even in the setting of multiple intra- and extracranial occlusions. 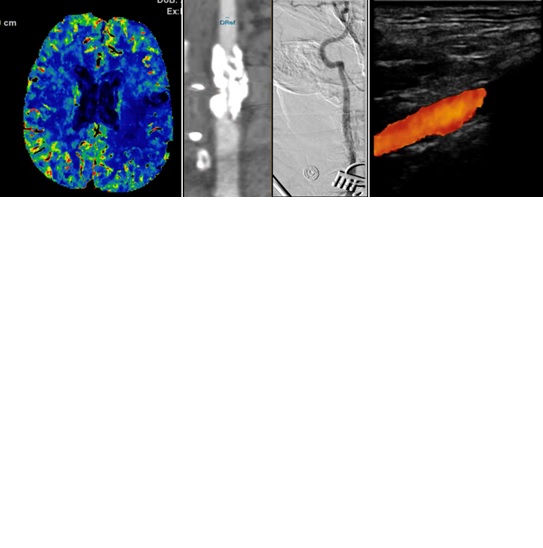
Back to 2020 Abstracts
