Complex Visceral Aneurysm Repair
Nida Ahmed, MD, Carlos Bechara, MD.
Loyola University Medical Center, Maywood, IL, USA.
DEMOGRAPHICS
52 year old male with history of hypertension and hypothyroidism.
HISTORY
Patient was admitted for campylobacter colitis and was incidentally found to have a 2cm aneurysm of the celiac artery extending into a 4.5cm right and left hepatic artery aneurysm. Patient completed two weeks of antibiotics for colitis prior to aneurysm repair to avoid graft infection. No history of trauma or vasculitis.
PLAN
Patient underwent laparotomy through a chevron incision. The supraceliac aorta was exposed. The liver was mobilized. A cholecystectomy was performed. The gastroduodenal artery was ligated. The supraceliac aorta was cross-clamped and an end-side anastomosis was created between the aorta and an 8mm Dacron graft. Blood flow was re-established to the liver. To avoid injury to the common bile duct, we elected to obtain distal control of the right and left hepatic arteries from within the aneurysm. The right hepatic artery was clamped proximally, maintaining blood flow into the left lobe of the liver. The aneurysm was opened and distal right hepatic artery control was achieved with a Fogarty balloon. An anastomosis was created to the Dacron graft. A second 8mm Dacron graft was sutured in an end-to-side fashion to the bypass. The side graft was clamped to re-establish flow to the right lobe of the liver. The left hepatic artery anastomosis was then created in the same fashion to the jump graft. After completion of anastomoses, there were excellent Doppler signals at each hepatic artery and the liver was well perfused. We then oversewed the splenic and common hepatic arteries.
DISCUSSION
This was a repair of a complex visceral aneurysm extending into the intrahepatic hepatic arteries. A transplant surgery surgeon was on standby for possible left hepatic resection. Multiple steps were taken to minimize liver ischemia time including maintaining flow to contralateral liver lobe during each hepatic anastomosis. Considering the depth of the anastomoses, a Dacron conduit was chosen over venous conduit to avoid kinking. The celiac artery aneurysm was 2cm but given the patientís young age, decision was made to address this aneurysm as well. Final pathology did not show evidence of infection. 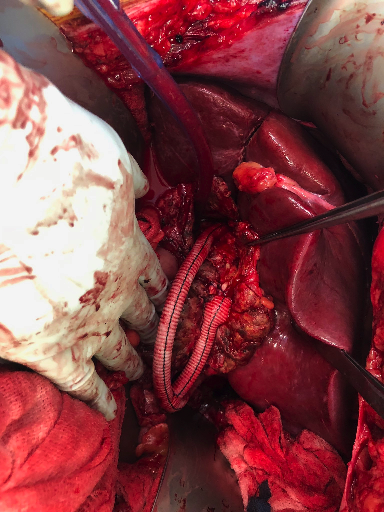
Back to 2020 Abstracts
