Management Of Acute Abdominal Aortic Occlusion With Resultant Profound Mesenteric And Renal Ischemia
Luis C. Cajas-Monson, MD, Manju Kalra, MBBS.
Mayo Clinic, Rochester, MN, USA.
DEMOGRAPHICS:
56-year-old female with ongoing nicotine dependence presented with acute abdominal pain and anuria.
HISTORY: Patient was transferred emergently with a 24-hour history of diffuse abdominal pain and anuria. She had been unwell for the preceding 2 weeks with emergency department visits for uncontrolled, symptomatic hypertension (270 mmHg systolic), and acute kidney injury (serum creatinine 2.6 from 0.8) but had refused treatment. She was in severe pulmonary edema, hyperkalemic (K 6.5), uremic (S. creatinine 3.8) and acidotic (pH 7.09) but hemodynamically stable and alert on arrival. Past history was significant for aortobifemoral and infrainguinal bypasses which had occluded and resulted in bilateral above knee amputations. Computed tomography angiography (CTA) revealed large, bilateral pleural effusions, occlusion of abdominal aorta, visteral and renal arteries, and infra-renal aortic graft.
PLAN: Patient was admitted directly to intensive care unit and hemodialysis immediately initiated. She was then transitioned to continuous replacement renal therapy (CRRT). After correction of hyperkalemia and improvement of acidosis, she was taken to operating room and maintained on CRRT intra-operatively. Diagnostic laparoscopy revealed global ischemia of bowel but no frank necrosis. Through a midline laparotomy, the supraceliac aorta was exposed and dissected into the posterior mediastinum to the patent segment. A low thoracic aortic clamp was placed and a longitudinal anterior aortomy was performed supraceliac. Fresh and chronic thrombus was extracted using endarterectomy spatula and inflow was established. A 12 x 6 x 7 x 6 mm trifurcated Dacron graft was anastomosed end-to-side with a long spatulated anastomosis. All limbs were tunneled retropancreatic and anastomosed to the superior mesenteric artery (SMA) and bilateral renal arteries. Immediately, the entire bowel pinked up and she started making copious amounts of urine. Abdomen was closed primarily. Post-operative course was uneventful with continuation of CRRT for 2 days for fluid removal. She was discharged home on post-operative day 15 in excellent condition.
DISCUSSION: Acute on chronic mesenteric and renal arterial occlusion is surprisingly well tolerated and can be resolved surgically with good outcomes. However, excellent physiologic and intestive care is simultaneously necessary and was achieved in this case with peri-and intra-operative CRRT to control homeostasis. 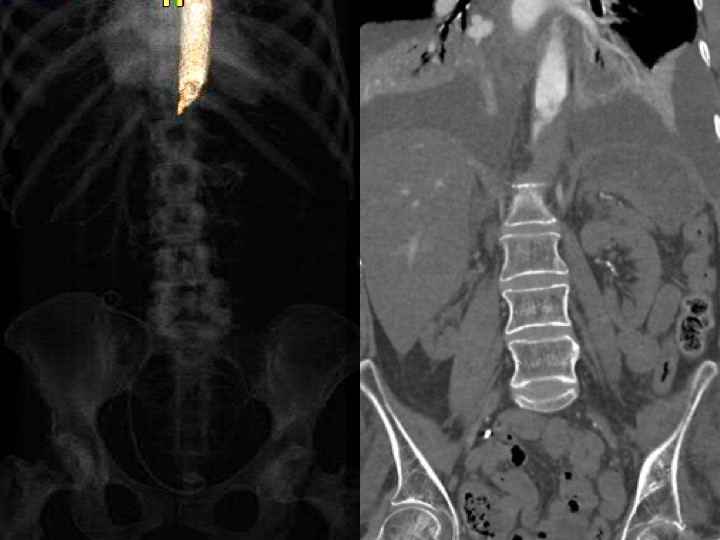
Back to 2020 Abstracts
