Ischemic Lumbosacral Plexopathy After Extensive Onyx Arterial Embolization For Type 2 Endoleak
Jaideep Das Gupta, M.D., Muhammad Ali Rana, M.D., Sundeep Guilani, M.D., John Marek, M.D..
University of New Mexico, Albuquerque, NM, USA.
DEMOGRAPHICS: Our patient is 63-year-old male who underwent extensive nonselective Onyx embolization for a type 2 endoleak and developed ischemic lumbosacral plexopathy. HISTORY: Our patient underwent an EVAR for a 6.1cm AAA. Fourteen-months post-operatively CT showed an aneurysm sac of 6.8cm with evidence of a type 2 endoleak arising from a patent inferior mesenteric artery (IMA) and lumbar arteries (Figure 1a).
PLAN: Arteriogram revealed a meandering mesenteric artery that retrograde filled a patent IMA and aortic sac. The aneurysm sac was unable to be cannulated and underwent coil embolization off the origin of the IMA. Completion arteriogram revealed placement of the coils (Figure 1b). Six-month CT scan showed enlargement of the aneurysm up to 7.3cm and persistent endoleak from lumbar arteries (Figure 1c). An arteriogram revealed a type 2 endoleak from the left iliolumbar arterial system; however was unable to cannulate the nidus within the sac. Coils were placed within the aneurysmal sac. Due to incomplete aneurysm seal, Onyx was then used for the intention to occlude the sac. Onyx liquid embolic agent was injected from the lumbar arteries into the sac and extensive non-target embolization within the iliolumbar arterial plexus occurred. Completion film showed placement of Onyx agent within nidus of aneurysm sac and extensive embolization of the lumbar arterial collateral circulation (Figure 1d). The patientís first neurological exam post-operatively was noted to have significant paresis of his hip flexors and knee extensors of his left leg, along with sensory deficits consistent with ischemic peripheral lumbosacral plexopathy. The patient was discharged to a rehab center on post-operative day 10 to continue physical therapy.
DISCUSSION: In our case, rather than direct access we were only able to indirectly access the aneurysmal sac and proceeded with Onyx injection. This w. as a judgmental error to administer extensive Onyx that lead to nonselective iliolumbar arterial embolization and for our patient resulted in ischemic lumbosacral plexopathy. Therefore, access the nidus for type 2 endoleaks and feeding vessels is paramount for effective treatment. This case underlines that extensive nonselective arterial liquid agent embolization of the iliolumbar arteries can lead to significant ischemic neurological injury. 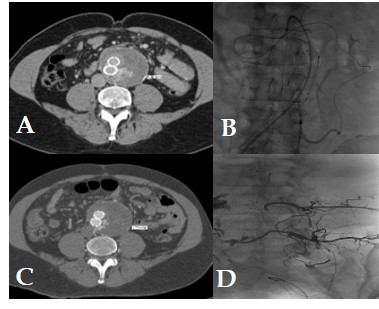
Back to 2020 Abstracts
