Trends In Use Of Cerebrospinal Drains And Outcomes Related To Spinal Cord Ischemia In The Vascular Quality Initiative
Victoria Aucoin, MD1, Bolanle Bolaji, MD, MPH1, Zdenek Novak, MD, PhD1, Emily Spangler, MD1, Graeme McFarland, MD1, Benjamin Pearce, MD1, Danielle Sutzko, MD1, Salvatore Scali, MD2, Adam Beck, MD1.
1University of Alabama at Birmingham, Birmingham, AL, USA, 2University of Florida, Gainesville, FL, USA.
Objective: Spinal cord ischemia (SCI) is a feared complication of aortic repair. We utilized the VQI database to identify trends in CSF drain usage in TEVAR and complex EVAR. We also sought to evaluate outcomes in patients who developed SCI despite preop drains vs those treated with therapeutic postop drains (ie selectively drained).
Methods: We evaluated elective TEVAR/cEVAR for aneurysm from 2014-2019 in the VQI; trauma, dissection and PAU/IMH were excluded. CSF drain use over time, factors associated with prophylactic vs therapeutic drain placement in those with any SCI (transient and/or permanent), and outcomes related to these groups were evaluated by χ2 analysis and Kaplan-Meier survival analysis.
Results: 3,469 TEVAR/cEVAR procedures met all criteria with an overall SCI rate of 2.5% (88/3469), which decreased from 4.55% in 2014 to 1.43% in 2018. Prophylactic drain use remained relatively stable (30% in 2014 to 27% in 2018); aortic coverage extent also remained consistent over time. Among the subset that developed SCI, demographics and prior history (including CAD, HTN, CHF, DM, CKD, and COPD) were not significantly different between the groups. Prior aortic surgery was significantly more common among patients with preop prophylactic drains compared to postop therapeutic (46.2% vs. 23%; p= .019). Procedure time was longer in patients requiring therapeutic drains for SCI compared to those with prophylactic drains developing SCI (mean 290 min vs. 183 min; p < .01). Total and postop lengths of stay were non-significantly longer with preop drain use. Survival analysis among SCI patients revealed decreased survival in patients who had postop therapeutic drains placed (Figure).
Conclusions: SCI rates decreased over time, although prophylactic CSF drain use has remained unchanged in the VQI. Among SCI patients, long-term survival was lower in patients with postop therapeutic drains placed compared to those who developed SCI with a preop prophylactic drain in place. Similar to MI or CVA where time to intervention for rescue matters, patients with therapeutic drains may fare worse than patients with prophylactic drains due to increased delays in decreasing CSF pressure leading to secondary spinal cord injury. This should give surgeons pause when considering a selective drain policy. 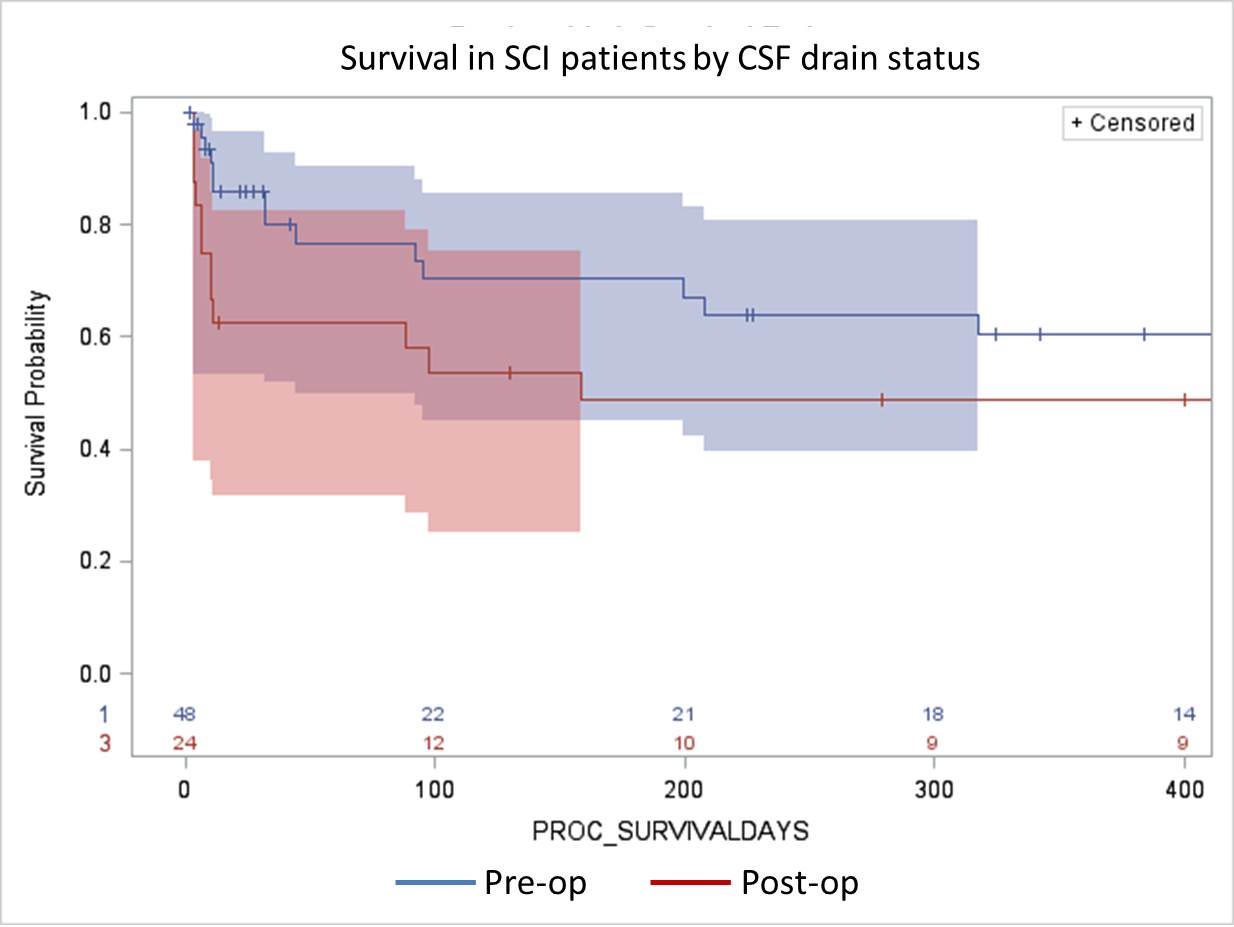
Back to 2020 ePosters
