Effect Of Symptom Type And Time From Symptom Onset On Outcomes Following Carotid Endarterectomy
Jinny J. Lu, MD, Chun Li, MD, Livia E.V.M. de Guerre, MD, Kirsten Dansey, MD, Ruby Lo, MD, Fahad Shuja, MD, Marc L. Schermerhorn, MD.
Beth Israel Deaconess Medical Center, Boston, MA, USA.
Objective: Current clinical practice and randomized controlled trials label patients with carotid territory symptoms >180 days prior to surgery as asymptomatic, however perioperative event rates may not be similar to patients who have never had symptoms. This study aims to determine the effect of symptom type and time since symptom on stroke/death following CEA. Methods: We utilized the VQI to identify patients undergoing primary, elective CEA from 2003-2019. These patients were divided into recently symptomatic (<180 days since symptoms), formerly symptomatic (>180 days), and asymptomatic cohorts. Recently symptomatic and formerly symptomatic patients were further subdivided by symptom-type: Stroke, TIA, and Amaurosis. Our primary outcomes were 30-day and 1-year stroke/death. Chi-square and multivariable logistic regression models were used for data analysis. Kaplan-Meier and Cox proportional hazard analysis were used for freedom from stroke/death analysis. Results: We identified 72,398 patients after exclusions: 16,997 (23.5%) were recently symptomatic, 2596 (3.6%) were formerly symptomatic, and 52,805 (72.9%) were asymptomatic. Overall, recently symptomatic patients had highest risk of 30-day stroke/death compared to formerly symptomatic, who had intermediate risk, and asymptomatic patients who were at lowest risk (3.3% vs 2.4% vs 1.5%, p<.01). Within the Stroke cohort, recently symptomatic patients had highest risk, formerly symptomatic had intermediate risk, and asymptomatic had lowest risk of 30-day stroke/death (3.7% vs 2.6% vs 1.5%, p<.01). Within the TIA cohort, only recently symptomatic patients had higher 30-day stroke/death rates (3.7% vs 1.5%, p<.01) compared to asymptomatic. Formerly symptomatic patients trended toward higher 30-day stroke/death rates (2.5% vs 1.5%, p=.07), but the difference was not significant. In Amaurosis patients, only recently symptomatic patients had higher 30-day stroke/death rates (2.1% vs 1.5%, p=.01) compared to asymptomatic patients. After risk adjusted Cox regression, 30-day freedom from stroke/death was not significantly different in formerly symptomatic patients compared to asymptomatic (HR 1.10 [0.79-1.53], p=0.57). At 1-year, freedom from stroke/death was significantly lower in formerly symptomatic patients compared to asymptomatic (HR 1.40 [1.21-1.62], p<.01).Conclusion: Patients presenting with stroke >180 days prior to elective CEA are at intermediate risk of stroke/death compared to recently symptomatic and asymptomatic patients. This should be factored into decision-making regarding treatment. 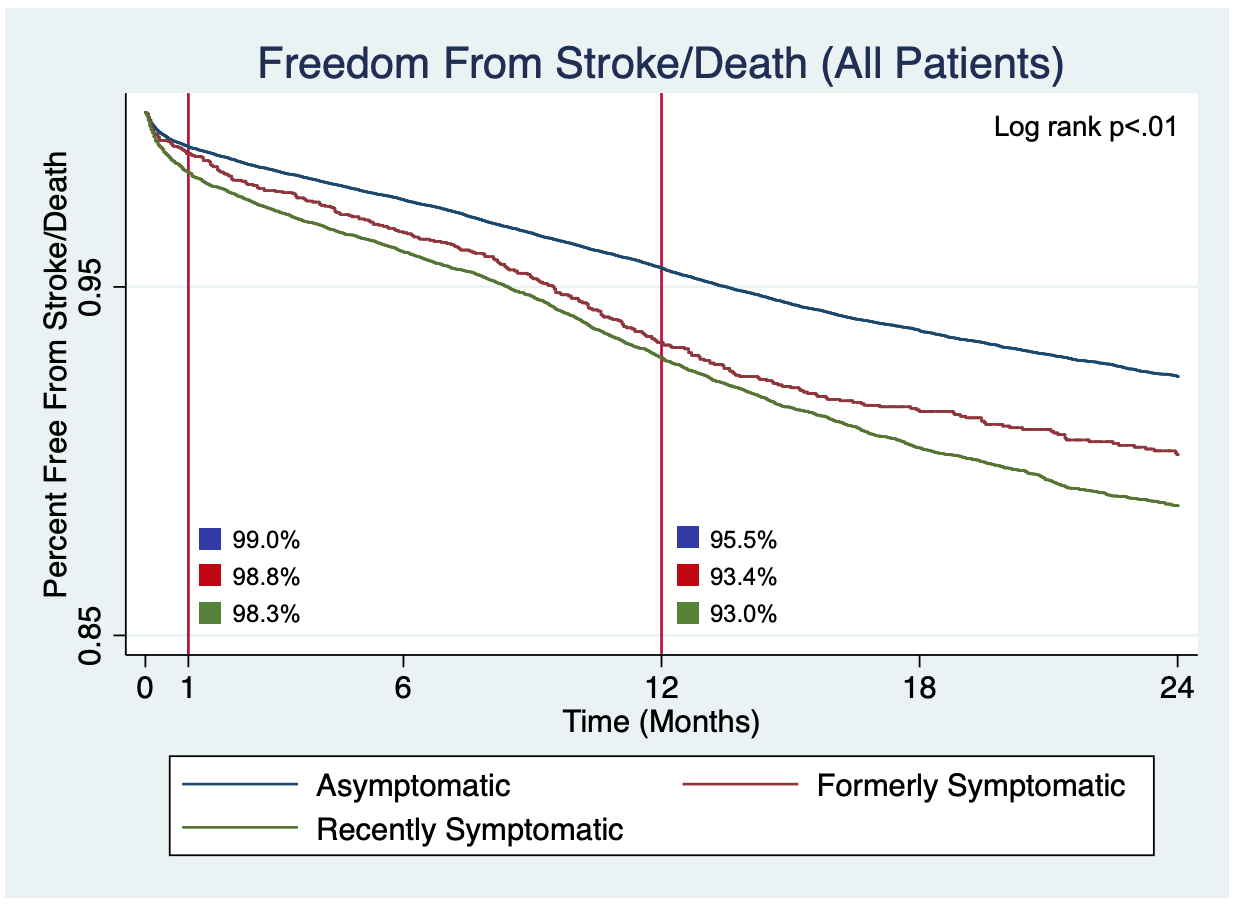
Back to 2020 ePosters
