Frailty Is Associated With Decline To Non-home Living Status After Vascular Surgery
Aditi Kashikar, MD1, Elizabeth L. George, MD1, Kara A. Rothenberg, MD2, Rui Chen, MS3, Nicolas B. Barreto, MPH3, Manjula Kurella Tamura, MD4, Amber W. Trickey, PhD, MS, CPH5, Philip Goodney, MD, MS6, Shipra Arya, MD, SM, FACS7.
1Department of Vascular Surgery, Stanford University School of Medicine, Stanford, CA, USA, 2Department of Surgery, University of California-San Francisco, East Bay, CA, USA, 3Stanford-Surgery Policy Improvement Research & Education Center, Department of Surgery, Stanford University School of Medicine, Stanford, CA, USA, 4Geriatric Research and Education Clinical Center, Veterans Affairs Palo Alto Healthcare System, CA, Stanford, CA, USA, 5Stanford-Surgery Policy Improvement Research & Education Center Department of Surgery, Stanford University School of Medicine, Stanford, CA, USA, 6Department of Surgery, The Dartmouth Institute, Lebanon, NH, USA, 7Department of Surgery, Stanford University School of Medicine, Stanford, CA, USA.
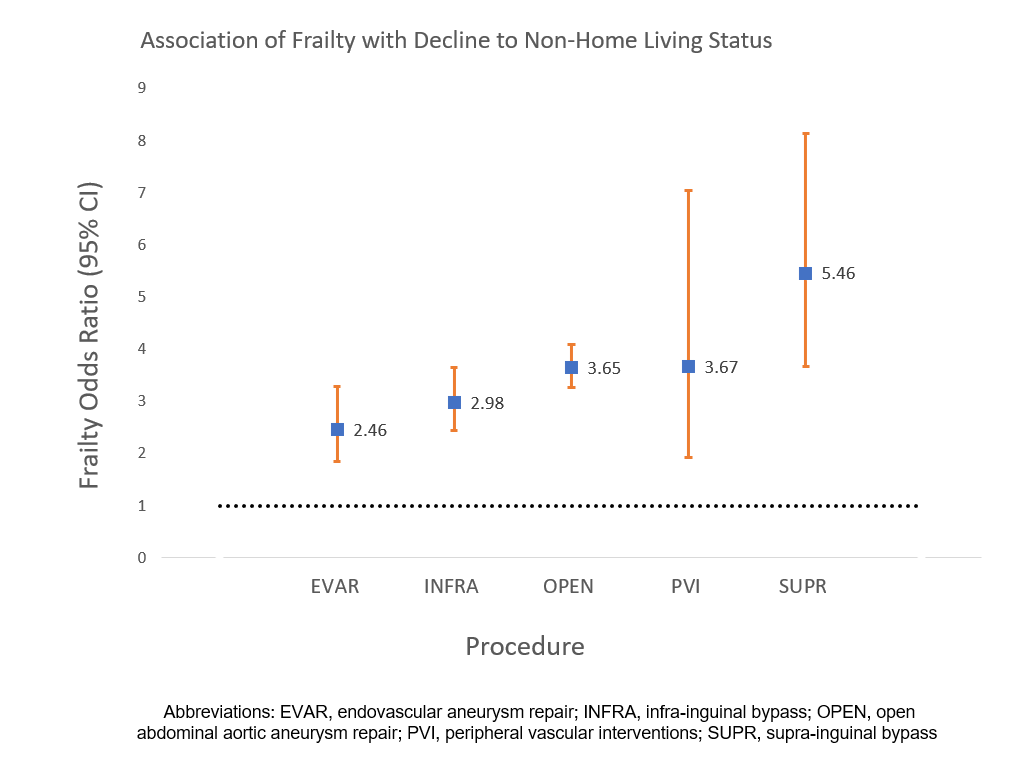
Objective There exists a knowledge gap in planning for long-term recovery and living status of patients undergoing vascular surgery. We explored associations of frailty with decline to non-home living status 1 year after abdominal aortic aneurysm (AAA) repair or peripheral artery revascularizations. Methods We utilized 2003-2017 Vascular Quality Initiative (VQI) data for home-dwelling patients undergoing AAA repair or peripheral artery revascularizations (EVAR, OPEN, SUPRA, INFRA, and PVI procedure files). Frailty was measured using the VQI-Risk Analysis Index (VQI-RAI) variables: gender, body mass index, kidney disease, congestive heart failure, dyspnea, living status, activities of daily living. Patients were classified as “frail” (RAI≥35) vs. “non-frail” (RAI<35) per prior work. Primary outcome was decline to non-home living at 1 year (± 3 months). Logistic regression models, stratified by procedure, were calculated to examine associations of frailty with decline to non-home living status. Results A total of 92,315 home-dwelling patients underwent vascular interventions: 56% (51,609) underwent initial peripheral vascular interventions (PVI); 19% (17,682) infra-inguinal bypass; 13% (11,678) endovascular AAA repair (EVAR); 4% (4,137) open AAA repair; and 8% (7,209) supra-inguinal bypass. Mean VQI-RAI score was 26.2 (SD 7.1), and 12,050 (13.1%) patients were classified as frail. Overall, 2,257 patients (2.4%) experienced postoperative decline to non-home living status at 1 year. Frail patients had higher odds of decline to non-home living status compared to non-frail patients, regardless of procedure (Figure). Frail patients had 2 times greater odds of decline to non-home living following EVAR (OR 2.46 [95% CI 1.85-3.28] p<0.001) and infra-inguinal bypass (2.98 [2.44-3.65] p<0.001). Frailty was associated with 3 times greater odds of decline to non-home living after PVI (3.65 [3.26-4.09] p<0.001) and open AAA (3.67 [1.92-7.04] p<0.001). After supra-inguinal bypass, frail patients had more than 5 times the odds of decline to non-home living (5.46 [3.67-8.14] p<0.001). Conclusions Frailty is significantly associated with decline to non-home living status in patients undergoing AAA repair or peripheral artery revascularizations, regardless of procedure. Preoperative frailty assessment could inform procedure-specific approaches to improve long-term functional recovery. Further research is needed to identify impact of decline in living status after surgery.
Back to 2020 ePosters
