Utilization Of Integrated Care In Patients With Concomitant Peripheral Artery Disease And Diabetes Is Low Overall And Differences Between Males And Females Are Small
Zachary J. Wanken, MD MS1, J. Aaron Barnes, MD1, Mark A. Eid, MD1, Niveditta Ramkumar, MPH2, Barbara Gladders, MS2, Andrea M. Austin, PhD1, Mark A. Creager, MD1, Mark P. Bonaca, MD MPH1, Mark W. Feinberg, MD1, Philip P. Goodney, MD MS1.
1Dartmouth-Hitchcock, Lebanon, NH, USA, 2The Dartmouth Institute for Health Policy and Clinical Practice, Hanover, NH, USA.
INTRODUCTION/OBJECTIVES: Integrated care strategies improve outcomes in patients with concomitant peripheral artery disease (PAD) and diabetes. At the same time, sex-based disparities in PAD care and outcomes are well established. This study examines utilization of integrated care strategies by sex in the largest contemporary patient sample to date.
METHODS: All Medicare claims, part A and B, from January 2003 until December 2016 were queried using previously validated diagnosis codes for PAD and diabetes. We defined integrated care by the completion of three tests: 1) vascular physiologic or imaging test, 2) serum hemoglobin a1c measurement, and 3) diabetic foot exam. Patients who received these tests within 6 months of PAD and diabetes diagnosis were identified and stratified by sex. To account for regional variation in preventive care practices, we compared sex-specific integrated care utilization rates across 307 Hospital Referral Regions (HRRs) using unpaired t-tests.
RESULTS: Over the study period, 10,506,254 Medicare patients with concomitant diagnoses of diabetes and PAD were identified. The overall prevalence for this combination of diagnoses was 15.3 per 1,000 Medicare patients during the study period. About half of these patients were female (52.7%, n=5,532,091). Of the three tests, patients were most likely to complete hemoglobin a1c exam (male 49.7%, female 49.4%) and were least likely to undergo diabetic foot exam (male 26.9%, female 32.9%). Across 307 HRRs, females were more likely to undergo hemoglobin a1c testing (51.7% vs 50.9%, p=0.02) and foot examination (30.7% vs 25.2%, p<0.001) whereas males were more likely to have a vascular imaging test (35.5% vs 34.4%, p<0.001). Figure 1 demonstrates variation across HRRs for each care modality stratified by sex.
CONCLUSIONS:
Among Medicare beneficiaries, males and females with concomitant diagnoses of PAD and diabetes were unlikely to undergo hemoglobin a1c testing, have a diabetic foot examination, and undergo an arterial imaging study. The between sex differences that we identified were small and ongoing initiatives should focus on increasing compliance with these tests for both males and females, particularly in low performing HRRs. 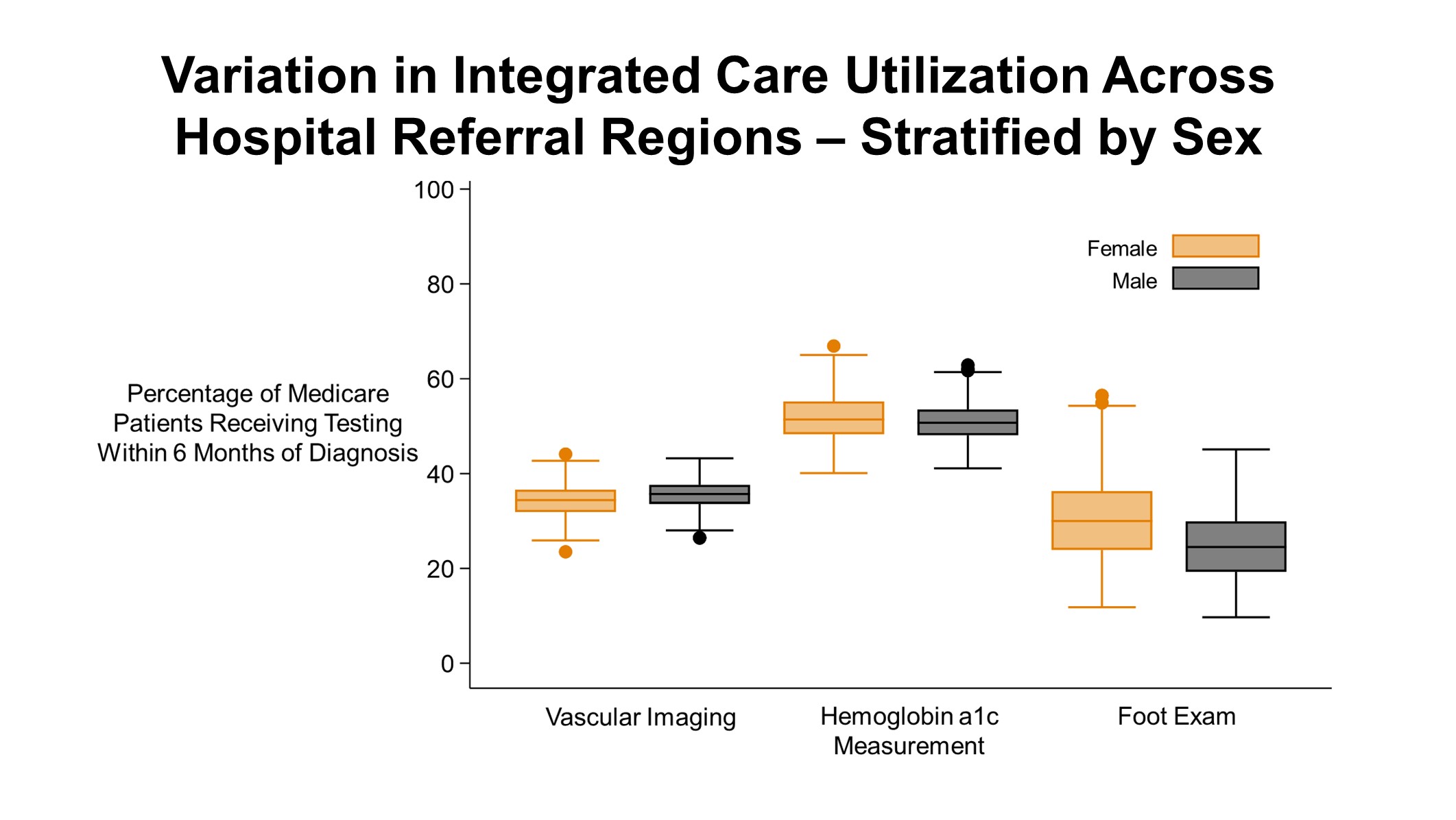
Back to 2020 ePosters
