Pancreaticoduodenal Artery True Aneurysms Near The Superior Mesenteric Artery: Endovascular And Surgical Treatment With Preservation Of Flow
Brittany C. Montross, MD, Elias Fakhoury, DO, Mariel Rivero, MD, Sonya Noor, MD, Linda M. Harris, MD, Sikandar Z. Khan, MD, Hasan H. Dosluoglu, MD.
University at Buffalo, Buffalo, NY, USA.
OBJECTIVE: Pancreaticoduodenal aneurysms (PDAA) are rare with only 100 reported cases to date, and repair is recommended independent of size due to high rupture risk and associated mortality. PDAA located near the SMA are particularly challenging and celiac artery stenosis is typically reported to be associated with pseudoaneurysms. We present three cases of electively repaired true PDAAs all associated with celiac artery occlusive disease while maintaining PDA flow.
METHODS: Retrospective review of patients' medical records undergoing open or endovascular repair of pancreaticoduodenal aneurysms within single vascular surgery department from 2016-2019.
RESULTS: Three patients (2 females, mean age 53) were diagnosed with saccular PDAAs by CTA, mean size 2.5cm. Two had celiac artery occlusion with large collateralization from the PDA to supply the liver. The third patient had celiac stenosis with post-stenotic dilatation and small common hepatic with significant filling via the gastroduodenal artery. All patients' aneurysm arose close to the origin of the PDA. One patient underwent endovascular coiling performed with balloon protection across the neck to prevent embolization. The other two patients had attempted transcatheter embolization which were unsuccessful. Resection of the aneurysm was performed and due to tortuosity the pancreaticoduodenal was transposed to the SMA, preserving the collateral pathway to the liver. Both patients had good flow noted distal to the anastomosis. (Figure 1). There were no ruptures in the interval period. Length of stay for endovascular was one day and 7 days for both open procedures.
CONCLUSIONS: Transcatheter embolization has recently been recommended as first-line treatment due to less invasiveness and good outcomes in patients whose anatomy permits. We found that often, due to the close proximity to the main SMA and complex tortuosity, embolization is not possible. Surgery with excision and reconstruction remains a valuable alternative in these patients, especially when PDA flow preservation is required.
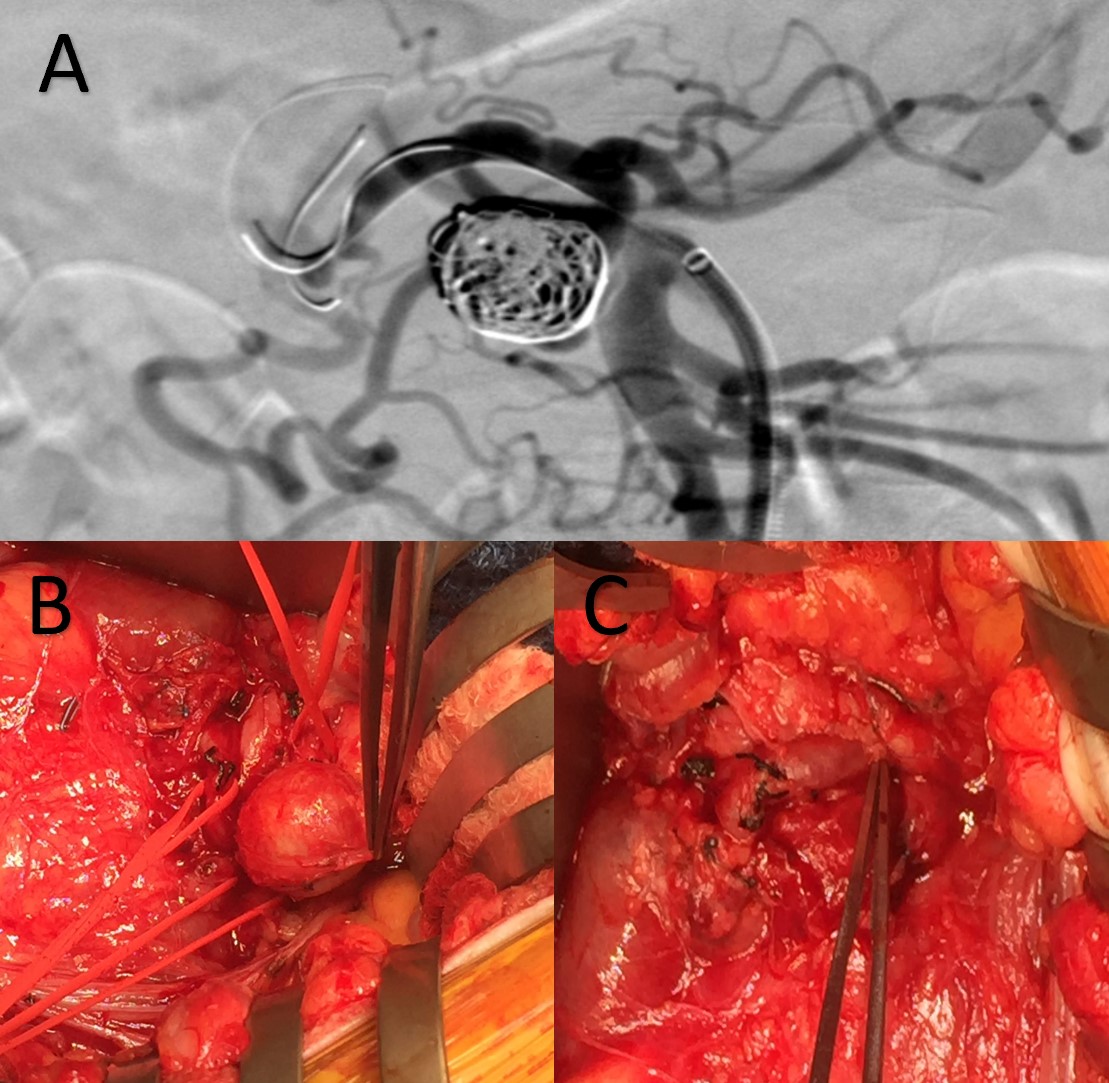
Figure 1: A) Coiled pancreaticoduodenal artery aneurysm, B) Pancreaticoduodenal artery aneurysm, C) Status post resection of aneurysm and transposition of pancreaticoduodenal
Back to 2020 ePosters
