Anticoagulation Therapy Adversely Affects Arteriovenous Access
Andrew E. Kumpfbeck, BA1, Caron B. Rockman, MD1, Glenn R. Jacobowitz, MD1, Neal S. Cayne, MD1, Michael E. Barfield, MD1, Andrew Lazar, MD2, Virendra I. Patel, MD2, Larry A. Scher, MD3, Karan Garg, MD1.
1NYU Langone Medical Center, New York, NY, USA, 2New York Presbyterian/Columbia University Medical Center, New York, NY, USA, 3Montefiore Medical Center, Bronx, NY, USA.
OBJECTIVES: Chronic anticoagulation (AC) use in patients with arteriovenous fistulas and grafts may be associated with increased risk of bleeding. The effects of AC on access patency and other complications is not well defined. Our goal was to assess the effect of anticoagulation use on outcomes after access creation.
METHODS: The Vascular Quality Initiative (VQI) database was queried for patients undergoing AVF creation or AVG, from 2011 to 2019. Anticoagulation use was defined as patients on Warfarin, Dabigatran, or Rivaroxaban, post access creation. Demographic and procedural details were analyzed. Wound infection and loss of patency within six months were assessed. Binomial logistic regression analysis was performed to assess the effect of anticoagulation use. RESULTS: We identified 27,757 AVF or AVG (21.2% and 78.8% respectively) patients with follow up data on long term anticoagulation use in the VQI. The average age was 61.4 years and 55.3% were male. 12.9% of patients were on AC, six months post access creation. The wound infection rate was 2.3% and 3.8% in no AC and AC cohorts, respectively (P <0.001). Loss of patency was 12.8% and 14% in the no AC and AC cohorts, respectively (P = 0.044). Grafts had higher loss of patency rates; those within the AC cohort had a loss of patency rate of 17.6% compared to 15.5% in the no AC group (P = 0.106). On multivariable analysis, anticoagulation use was associated with higher risk of wound infections (odds ratio [OR] 1.60, 95% confidence interval [CI] 0.987-1.312, P = 0.001). Although AC use did not significantly affect access patency, there was a trend towards an increased rate of patency loss (OR 1.138, 95% CI 0.987-1.312, P = 0.075).
CONCLUSIONS: Long term anticoagulation was associated with a higher wound infection rate, and may increase access thrombosis. AC use in patients with hemodialysis access appears to offer no clinical benefit and may be associated with worse outcomes. 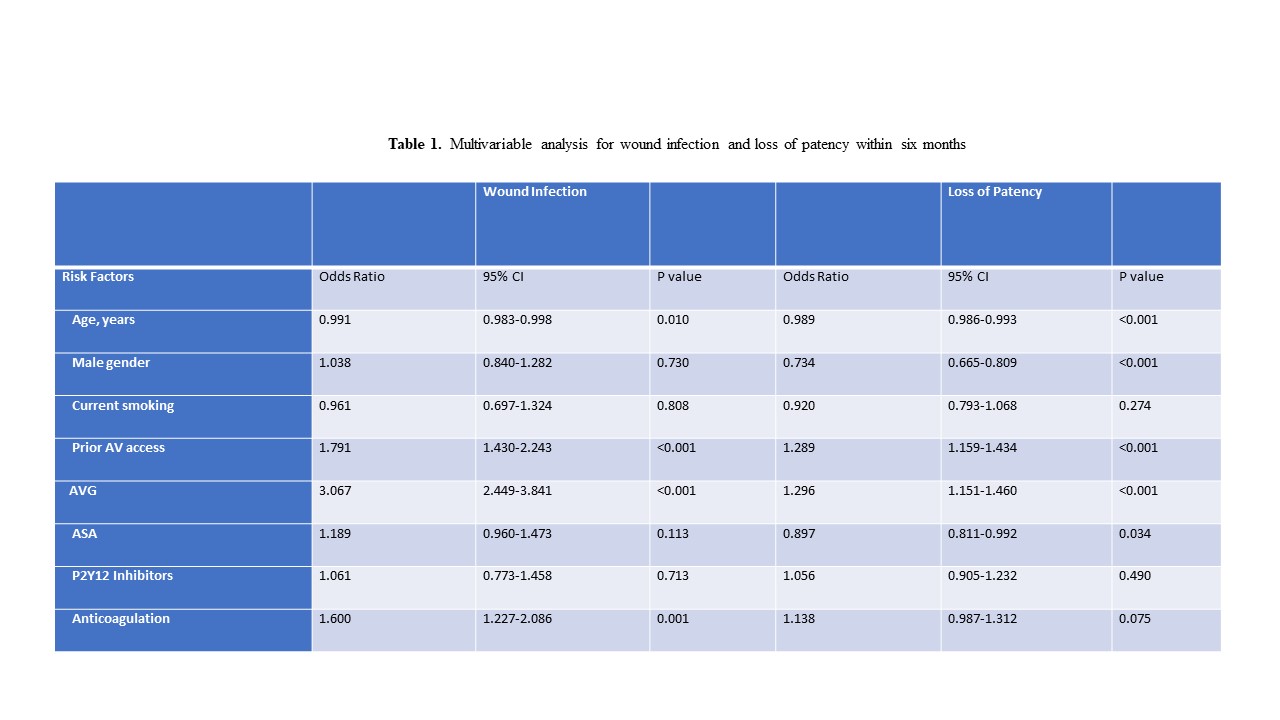
Back to 2020 ePosters
