Outcomes Of Upper Extremity Arterial Bypass For Trauma
Hunter M. Ray, MD, Daniel G. Miles, MD, Samuel D. Leonard, MD, Charles C. Miller, III, PhD, Harleen K. Sandhu, MD, MPH, David E. Meyer, MD, Naveed U. Saqib, MD, Kristofer M. Charlton-Ouw, MD.
The University of Texas Health Science Center at Houston, McGovern Medical School, Houston, TX, USA.
OBJECTIVES:
Trauma remains a leading cause of morbidity and mortality worldwide. Vascular injuries are present in roughly 1% to 2% of trauma patients, with the majority of injuries occurring to the extremities. This study aimed to determine predictors of poor outcomes in upper extremity bypasses performed for traumatic arterial injury.
METHODS:
All patients admitted between November 2002 and October 2017 who underwent upper extremity arterial bypass for trauma at a single level 1 trauma center were included for analysis. The primary outcome was a composite of revision for bleeding or thrombosis, arm amputation or perioperative death. Data were analyzed by frequency and contingency table analysis with Kaplan-meier methods utilized for survival analysis.
RESULTS:
During the Study period 31 patients presented with upper extremity arterial injuries and underwent arterial bypass. The cohort mean age was 27.2±13.5 years (median:25 years); 81% male. The mechanism of injury was penetrating in 20/31 (64.5%) with the remaining having a blunt mechanism. Specialty performing the bypass was Vascular surgery in 22/31(71%), with the remainder by Trauma, Plastics or Pediatric surgery. Autologous vein was used in 29/31(93.5%). No significant predictors of poor outcome were noted including penetrating versus blunt mechanism (p=0.18), specialty performing bypass(p=0.98), interposition bypass(p=0.64), associated orthopedic injury(p=0.35), injury severity score [ISS](p=0.31), and type of conduit used (p=0.34). Overall the composite outcome was reached in only 7/31 patients with this low event rate likely contributing to the inability to determine specific predictors of poor outcome. Follow-up demonstrates 90% survival at 20 months. (Figure1)
CONCLUSIONS:
Upper extremity bypass for traumatic arterial injury has a low event rate using a composite endpoint. While this may be an effect of sample size it appears that these patients do well overall. Larger datasets are needed to determine predictors of outcome in a population with a relatively low event rate. 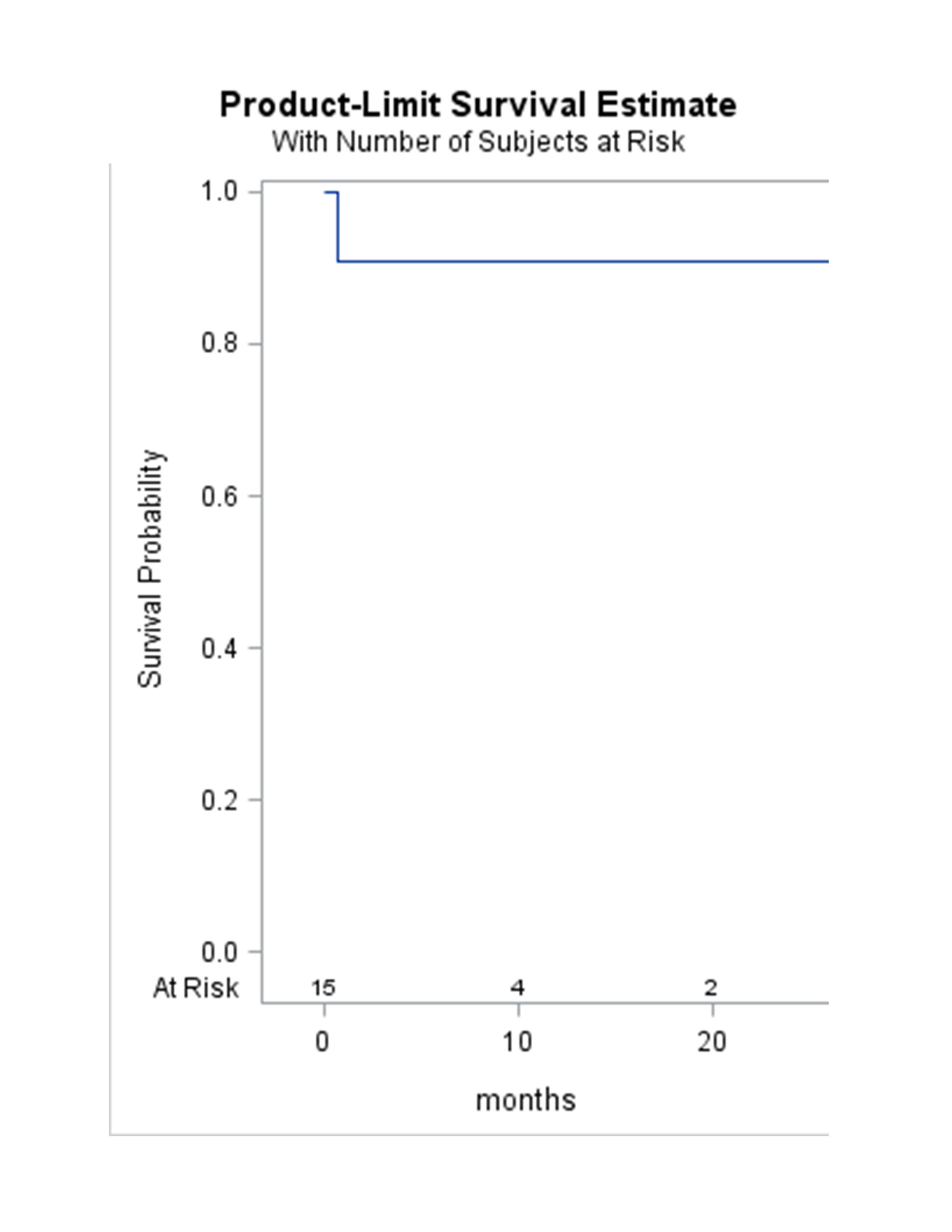
Back to 2020 ePosters
