Median Arcuate Ligament Syndrome: A Single-Center Experience With Laparoscopic Release Alone
Kevin C. Eddinger, MD, Jordan B. Stoecker, MD, David Horak, Daniel T. Dempsey, MD, Paul J. Foley, III, MD, Kristoffel R. Dumon, MD, Benjamin M. Jackson, MD.
Hospital of the University of Pennsylvania, Philadelphia, PA, USA.
OBJECTIVES: Median arcuate ligament syndrome (MALS) is a poorly-understood clinical entity thought to arise from anatomic compression of the celiac artery or celiac plexus by the median arcuate ligament. Patients complain of inconsistent abdominal symptoms, and frequently undergo extensive workups across multiple medical subspecialties. Surgical treatment involves division of the median arcuate ligament with or without stenting of the celiac axis. Stent placement commits patients to long-term follow-up and increases potential for complications. We sought to characterize patient outcomes after minimally invasive ligament release without endovascular intervention.
METHODS: All patients who underwent laparoscopic median arcuate ligament release at a single institution were identified and included in this retrospective case series. Data is expressed as mean ± standard deviation unless noted.
RESULTS: A total of 22 patients underwent median arcuate ligament release between 2015 and 2019. None underwent celiac stenting. Patient demographics are summarized in Table 1. Patient age was 45 ± 20 years (range 16-79). There were 15 females (68%) and 7 males (32%). Preoperative BMI was 28 ± 9 kg/m2. Nine patients had co-existing pain conditions (41%), and six were on narcotics preoperatively (27%). All patients had CTA or MRA evidence of celiac artery compression by the median arcuate ligament. The most common symptoms were: post-prandial abdominal pain (86%), constant abdominal pain (68%), and nausea or emesis (68%). Median duration of symptoms was 12 months. Twelve patients reported unintentional weight loss (54%) averaging 15 ± 12 lb. There was one intraoperative conversion to laparotomy for bleeding not requiring blood transfusion (4.5%). Hospital length of stay was 1.9 ± 1.2 days. At initial follow-up, twenty patients reported complete resolution of their presenting symptoms (91%), while two continued to experience a milder form of these symptoms (9%). Initial symptoms recurred in an additional three patients (14%) after a median interval of one month. Three subsequently developed new abdominal symptoms different from their preoperative symptoms (14%). Fourteen remained without symptoms at their last follow-up (64%).
CONCLUSIONS: Laparoscopic median arcuate ligament release for MALS without endovascular intervention is both safe and effective in select patients, and does not require long-term surveillance or maintenance. 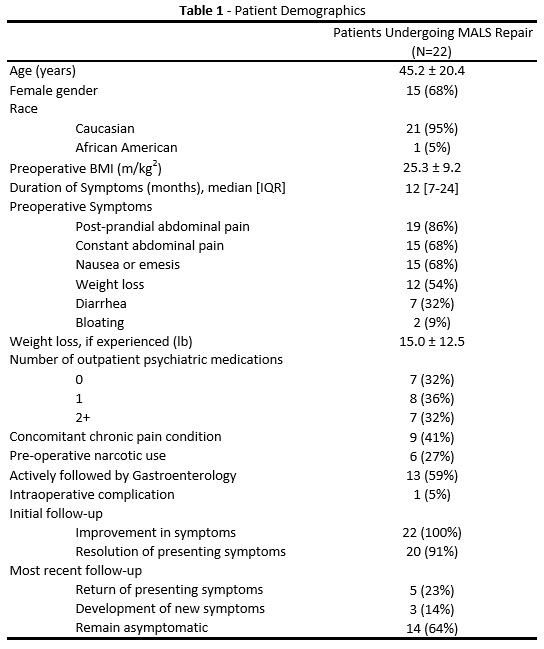
Back to 2020 ePosters
