Failure To Rescue Following Complications Is More Common After Open Repairs Of Larger Infrarenal Aneurysms
Ambar Mehta, MD, MPH1, Tania Torres-Sanchez, MD1, Richard W. Schutzer, MD1, James Iannuzzi, MD, MPH2, Jeffrey Siracuse, MD3, Karan Garg, MD4, William D. Clouse, MD5, Virendra I. Patel, MD, MPH1.
1Columbia University Medical Center, New York, NY, USA, 2UCSF School of Medicine, San Francisco, CA, USA, 3Boston University Medical Center, Boston, MA, USA, 4NYU Langone Medical Center, New York, NY, USA, 5University of Virginia, Charlottesville, VA, USA.
OBJECTIVES: Operative experience, clinical intuition, and prior research dictate that larger infrarenal abdominal aortic aneurysms have worse postoperative outcomes after open repairs. Understanding the clinical mechanisms underlying this association can inform quality improvement initiatives to reduce adverse outcomes. In this study, we evaluated rates of complications and failure-to-rescue (death after a major postoperative complication) by maximum aneurysm diameter among patients undergoing open repairs of infrarenal aneurysms.
METHODS: In the 2004-2018 Vascular Quality Initiative, we identified all patients undergoing open repairs of non-ruptured infrarenal aneurysms. Primary outcomes included 30-day mortality, complications, and failure-to-rescue. Secondary outcomes included cardiac, pulmonary, and renal complications, with their respective rates of failure-to-rescue. We used multilevel logistic regressions, clustered at the hospital level, to adjust for confounding when examining each outcome, with aneurysm diameter as the independent variable (unit: one-centimeter).
RESULTS: We identified 4192 patients (median age 69 years, 75% male, 91% Caucasian), where the median aneurysm diameter was 5.6cm (IQR 5.2-6.5cm). Overall, 30-day mortality was 3.3%, complications were 33.1%, and failure-to-rescue was 9.1%. For every one-centimeter increase in aneurysm size, the adjusted odds of 30-day mortality increased by 20% (OR 1.20, 95%-CI 1.09-1.33), remained similar for complications (OR 1.02, 95%-CI 0.98-1.07), and increased again for failure-to-rescue by 22% (OR 1.22, 95%-CI 1.07-1.38). Repeating these analyses by specific complications revealed similar findings (Table), where one-centimeter increases in aneurysm diameter were not associated with the prevalence of either renal, cardiac, or pulmonary complications. However, incremental aneurysm diameters by one-centimeter were associated with higher rates of failure-to-rescue among patients who experienced renal and cardiac complications.
CONCLUSIONS: Larger infrarenal aneurysms have higher postoperative mortality rates after open repairs due to greater rates of failure-to-rescue, not overall complications. Specifically, renal and cardiac complications have the highest rates of failure-to-rescue. Establishing system-level initiatives, creating unit cultures, and developing hospital-specific protocols can improve patient outcomes by decreasing the time to identifying a postoperative complication and standardizing initial treatment pathways. 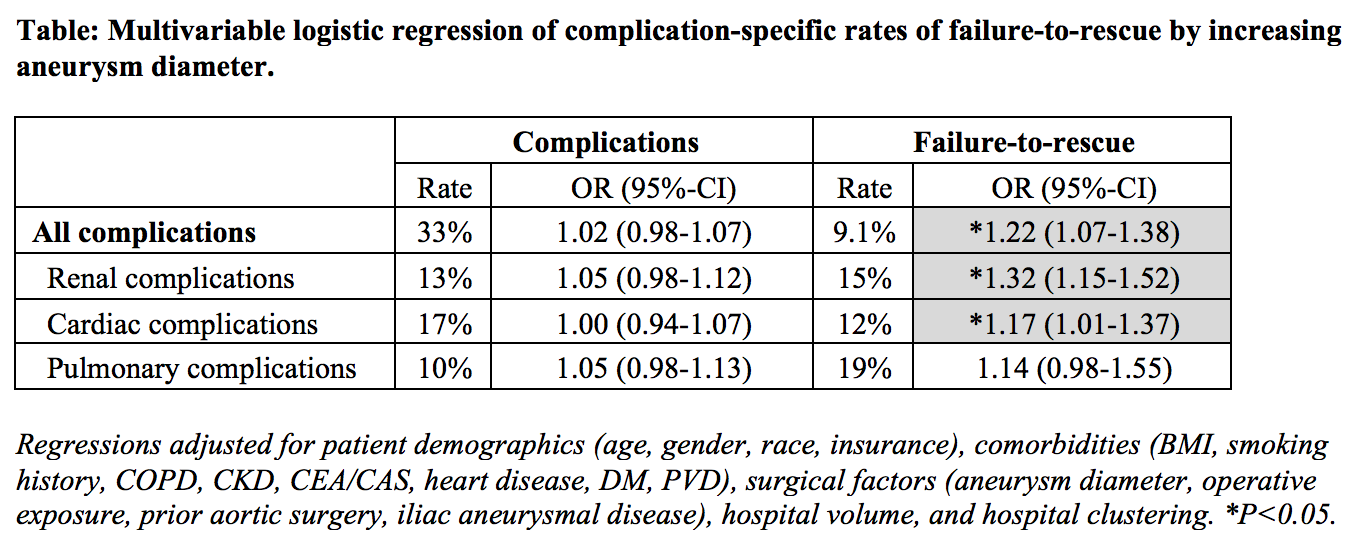
Back to 2020 ePosters
