Increased Utilization Of Dual Antiplatelet Therapy After Lower Extremity Bypass Surgery Without Increased Graft Patency
Nathan Belkin, MD, Jordan B. Stoecker, MD, Paul J. Foley, MD, Scott M. Damrauer, MD, Benjamin M. Jackson, MD, Ronald M. Fairman, MD, Grace J. Wang, MD.
Hospital of the University of Pennsylvania, Philadelphia, PA, USA.
Objective:
Current guidelines recommend single agent antiplatelet therapy for patients with symptomatic PAD and for consideration of dual antiplatelet therapy (DAPT) after surgical revascularization. The objective of this study was both to explore prescribing patterns of single versus dual antiplatelet therapy after lower extremity bypass surgery, and to investigate the effects of antiplatelet therapy on bypass graft patency.
Methods:
A retrospective review of non-emergent infra-inguinal lower extremity bypass operations entered in the national Vascular Quality Initiative (2003-present) was performed. Patients discharged on aspirin monotherapy or dual antiplatelet therapy with aspirin and a second agent (DAPT) were identified. Linear regression investigated temporal trends in antiplatelet utilization. Multivariable Cox regression investigated predictors of primary, primary-assisted, and secondary patency.
Results:
Of the 13,020 patients investigated, 52.2% were discharged on aspirin monotherapy, and 47.8% on DAPT. The proportion of patients discharged on DAPT increased from 8.5% in 2003 to 64.3% in 2019 (P<0.001, Figure), due to increased utilization of clopidogrel and other novel antiplatelet agents. Patients discharged on DAPT were younger, more often female, had higher rates of medical comorbidities (HTN, diabetes, CAD, CHF, COPD), and had higher rates of prior lower extremity and coronary interventions. The DAPT cohort had higher risk operative features with more distal targets and more frequent prosthetic conduit utilization. Tibial bypass target (HR 2.06, 95%CI 1.56-2.72, P<0.001), non-autologous conduit (HR 1.88, 95%CI 1.50-2.36, P<0.001), spliced vein conduit (HR 1.34, 95%CI 1.12-1.62, P=.002), more advanced presenting symptoms (HR 1.62, 95%CI 1.13-2.31, P=0.009), prior lower extremity intervention (HR 1.22, 95%CI 1.09-1.36, P<0.001), and female gender (HR 1.20, 95%CI 1.11-1.28, P<.001) were associated with diminished primary patency. DAPT had no additive benefit over aspirin with primary (HR 0.98, 95%CI 0.88-1.10, P=0.78), primary assisted (HR 0.93, 95%CI 0.80-1.07, P=0.33) or secondary patency (HR 0.88, 95%CI 0.74-1.06, P=0.19).
Conclusions:
A significant and increasing proportion of patients are discharged on dual antiplatelet therapy after lower extremity bypass revascularization. These patients represent a higher risk cohort with more medical comorbidities and higher risk bypass features. Despite its increasing utilization, DAPT therapy provided no additional benefit over aspirin on graft patency after lower extremity bypass surgery. 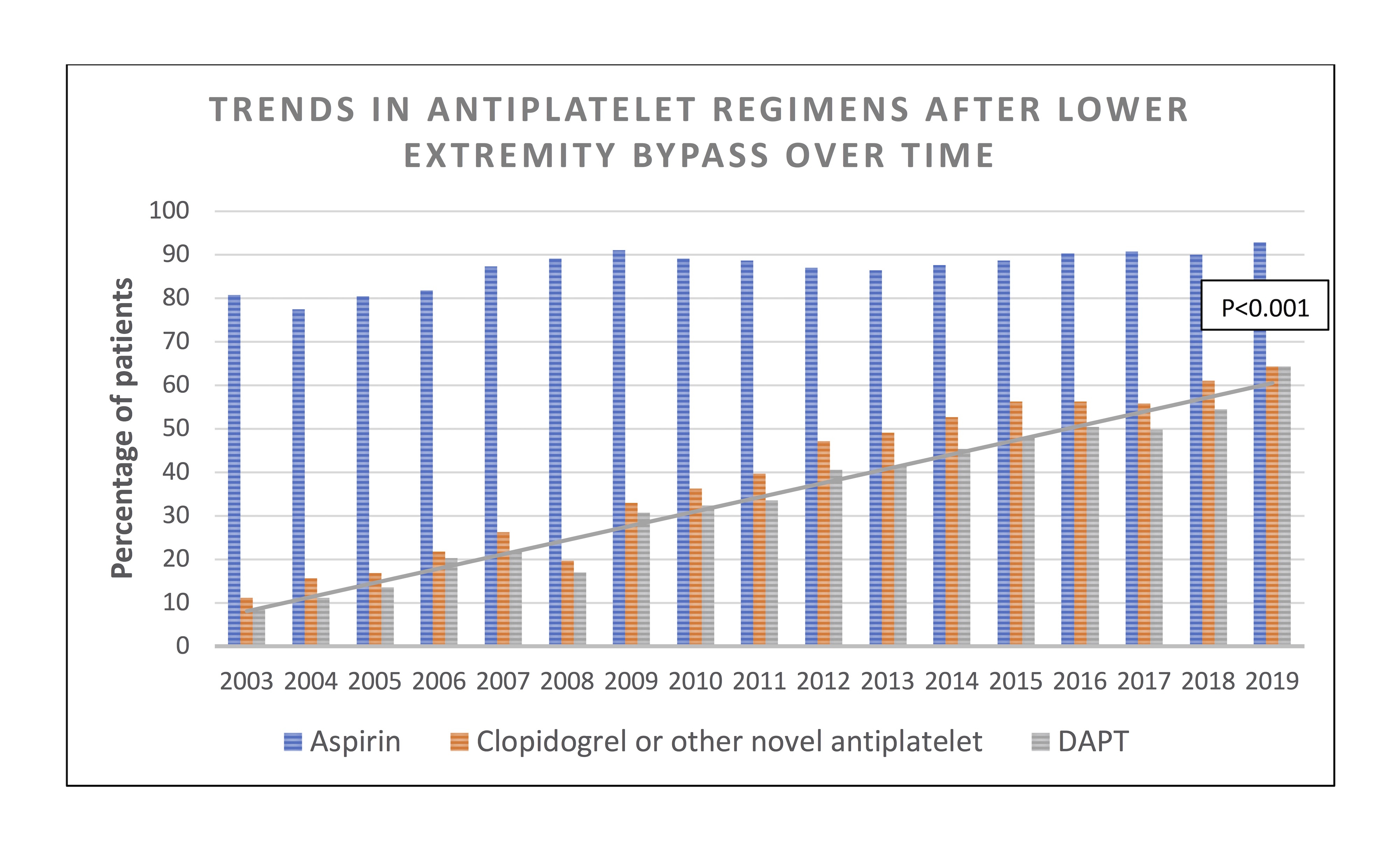
Back to 2020 ePosters
