Patient And Procedural Factors Affecting Outcomes Of Contemporary Endovascular Therapy For Femoral-Popliteal Atherosclerotic Disease
James D. Reese, M.S., Animesh Rathore, M.D., Andrew F. McChesney, M.D., Anand Dayama, M.D., Michael A. Corbin, Justin M. Milligan, M.D., Limael E. Rodriguez, M.D., Samuel N. Steerman, M.D., David J. Dexter, M.D., Jean M. Panneton, M.D..
Eastern Virginia Medical School, Norfolk, VA, USA.
OBJECTIVES: The factors affecting outcomes of endovascular revascularization have not been well described on a large scale. We aim to report risk-factors associated with loss of primary patency, major amputation, and mortality for patients undergoing de-novo endovascular revascularization for femoral-popliteal lesions.
METHODS: Retrospective review of patients undergoing de-novo endovascular revascularization of the femoral-popliteal arteries at a large academic vascular practice between January 2010 and December 2018 for atherosclerotic lesions was performed. Patients with claudication or chronic limb-threatening ischemia (CLTI) were included. Demographics, comorbidities, Rutherford score, and lesion characteristics were collected. Primary endpoints were loss of primary patency, major amputation, and all-cause mortality. Data analysis with SPSS (IBM; Armonk, NY) was performed using X2 and ANOVA tests.
RESULTS: 521 patients were evaluated. Mean age was 66.8 (±10.9) years, and 44.5% were female. Mean BMI was 28.0 (±5.9) kg/m2. Incidence of hypertension was 86.8%, diabetes was 53.6%, end-stage renal disease (ESRD) was 9%, coronary artery disease (CAD) was 40.5%, and past or current tobacco use was 85%. Mean pre-op ankle-brachial index (ABI) was 0.59 (±0.19) and median Rutherford score was three. 59.5% had loss of at least 1 tibial vessel runoff. Atherectomy was used in 256 procedures, drug-coated balloons (DCB) in 232, and stents in 139. Two-year primary patency, major amputation for patients with tissue loss, and mortality rates were 39.3%, 14.8%, and 8.6%, respectively. Superior primary patency rates were associated with DCB use (72.4% vs. non-DCB 45.3%; p<0.001) and pre- to post-op ABI change of >0.15 (63.1% vs. change <0.15; 45.2% p=0.003). Major amputation was associated with ESRD (14.9% vs. 3.0%; p<0.001) and CAD (7.6% vs. 1.6%; p=0.001). Mortality was associated with ESRD (23.4% vs. 7.9%; p<0.001), chronic heart failure (22.6% vs 7.5%; p<0.001), CAD (14.4% vs. 5.8%; p=0.001), and major amputations (23.8% vs. 8.7%; p=0.019). Mortality was not significantly impacted by DCB use (8.2% vs. 10.1%; p=0.45).
CONCLUSIONS: This study evaluates the patient and procedural factors affecting outcomes in patients undergoing primary endovascular revascularization for atherosclerotic femoral-popliteal lesions. Acceptable limb salvage was experienced with primary endovascular approach in patients with tissue loss. DCB use was not associated with increased short-term mortality. 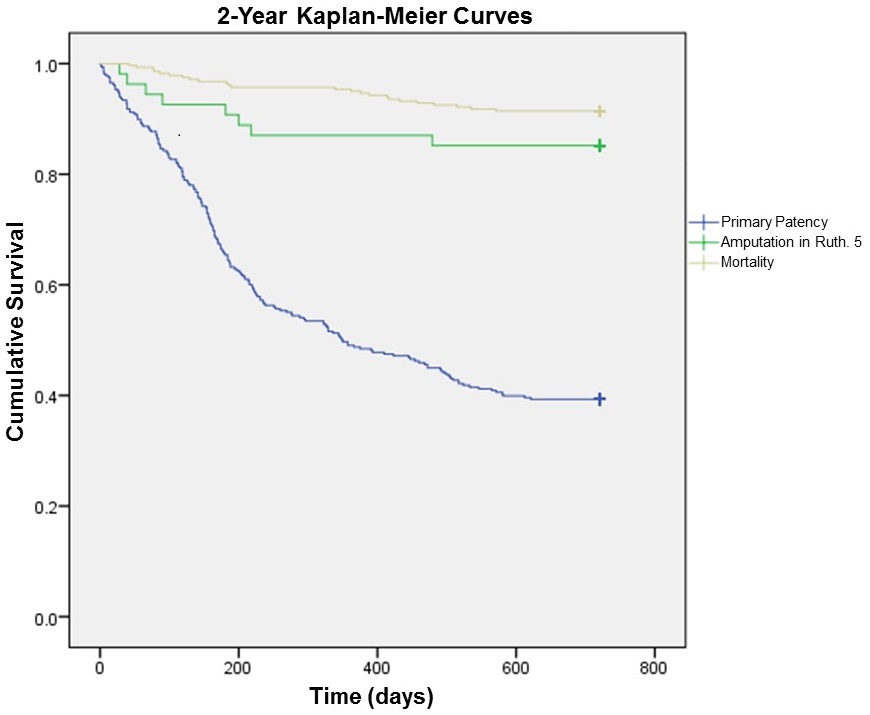
Back to 2020 ePosters
