Drug-eluting Stent Vs. Bypass For Femoro-popliteal Occlusive Disease
Asma Mathlouthi, M.D, Hanaa Dakour-Aridi, M.D, Omar Al-Nouri, M.D, Mahmoud B. Malas, M.D, M.H.S.
University of California, San Diego, San Diego, CA, USA.
OBJECTIVES: Numerous studies have compared the outcomes of bypass and bare-metal stent in the management of femoro-popliteal occlusive disease. However, the available evidence has become scarce since the advent of drug-eluting stents(DES). The aim of this study is to compare the mid-term, real-world outcomes of DES and bypass for treating femoro-popliteal occlusive disease.
METHODS: We identified all patients who underwent femoro-popliteal revascularization at our institution from January 2012 to December 2017. We selected all patients who received drug-eluting stenting or bypass using autogenous vein. We compared the primary patency, overall survival and limb salvage at two years between the two groups. A comparison between the two groups within Trans-Atlantic Society Consensus(TASC)II subgroups was also performed. Multivariate Cox regression models were used to examine the treatment effect on the main outcomes.
RESULTS: Of the study cohort, 129 patients(56.1%) received femoro-popliteal bypass, while 101 patients(43.9%) underwent DES placement. Median follow-up time was 19 months(IQR 11-29). Patients in the DES group were more likely to have TASC A and B lesions(77.2%), whereas 63% of patients in the bypass group had TASC C and D lesions. The overall 2-year primary patency estimates were 82.1% for the DES group compared to 59.2% for the bypass group(P<0.001). After adjusting for age, gender, comorbidities and TASC, bypass use was associated with greater than 2-fold increase in loss of primary patency[aHR(95%CI): 2.6(1.3-5.1), P=0.05]. There were no differences in the 2-year overall survival(88.1% vs 87.8%) and limb salvage(92.5% vs 92%) between the DES and the bypass groups, respectively. These findings persisted among patients with TASC A and B lesions. However, in TASC C and D patients, there was a trend towards decreased survival with DES compared to bypass (77.6%vs88.8%,P=0.1).
CONCLUSIONS: The use of DES in a real world setting was associated with a higher primary patency among patients with TASC A and B lesions, , whereas bypass did not offer an advantage in terms of patency in longer lesions (TASC C and D). Interestingly, a trend towards a higher mortality after DES placement in patients with TASC C and D lesions was noted. Further studies of larger populations are required. 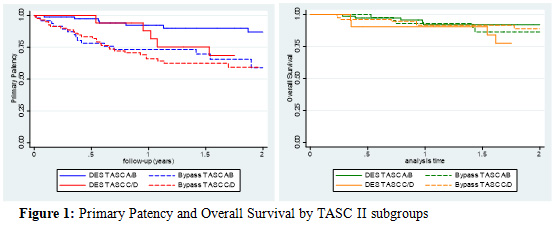
Back to 2020 ePosters
