A Staged, Hybrid Approach For The Treatment Of Complex Type II And III Thoracoabdominal Aortic Aneurysms
Adam Tanious, MD, MMSc, Elizabeth Chou, MD, Laura T. Boitano, MD, MPH, Lauren Canha, BS, Christopher Latz, MD, MPH, Matthew Eagleton, MD, Samuel Schwartz, MD, Mark F. Conrad, MD, MMSc.
Massachusetts General Hospital, Boston, MA, USA.
Introduction:
Open repair of type II and III thoracoabdominal aneurysms (TAAA) is reserved for healthy patients and the availability of totally endovascular repair is limited to select institutions. A staged, hybrid approach using thoracic endografting (TEVAR) in the descending thoracic aorta followed by open repair of the visceral and infrarenal aorta that incorporates the distal endograft in the proximal suture line is an alternative option for some patients. This study details our results with this approach.
Methods:
All patients who underwent a staged, hybrid repair of type II and III TAAA’s from 2006 – 2018 were identified. Analysis was performed of demographic, operative, and outcomes variables.
Results:
Eight patients were identified in the cohort. Demographic and peri-operative data are summarized in Table 1. The majority of patients received spinal drains for the TEVAR (n=6, 75%), and 3 patients required left subclavian artery coverage. Graft upsizing at the proximal attachment site averaged 23% (+/- 10%) and most patients had 3 grafts placed with distal landing in zone 9 for in 75% of cases.
Technical success of the TEVAR was achieved in 100% of cases. The median time between the TEVAR and open repair was 140 days (IQR=43 - 311 days). The median effect of TEVAR on sac diameter was a 0.7cm decrease in size (IQR= -1.9 – 0.6cm) over the entirety of follow-up. The average length of stay after TEVAR was 9 days (+/- 4.5 days). Five patients (63%) experienced at least one post-operative complication, and 2 required a secondary intervention for endoleak. There was no in-hospital mortality after TEVAR and only 1 in-hospital death after open repair. With a median follow-up of 1.7 years (IQR=0.9 – 3.5 years), 75% of patients experienced sac stability/regression with no patient lost to follow-up. Unadjusted survival at 1-year was 67%.
Conclusion:
A staged, hybrid approach using TEVAR in the descending thoracic aorta followed by open aortic repair that incorporates the distal endograft in the proximal suture line can be accomplished with a high degree of technical success. This repair strategy also has positive effects on aortic remodeling with 75% of patients experiencing sac regression/stability. 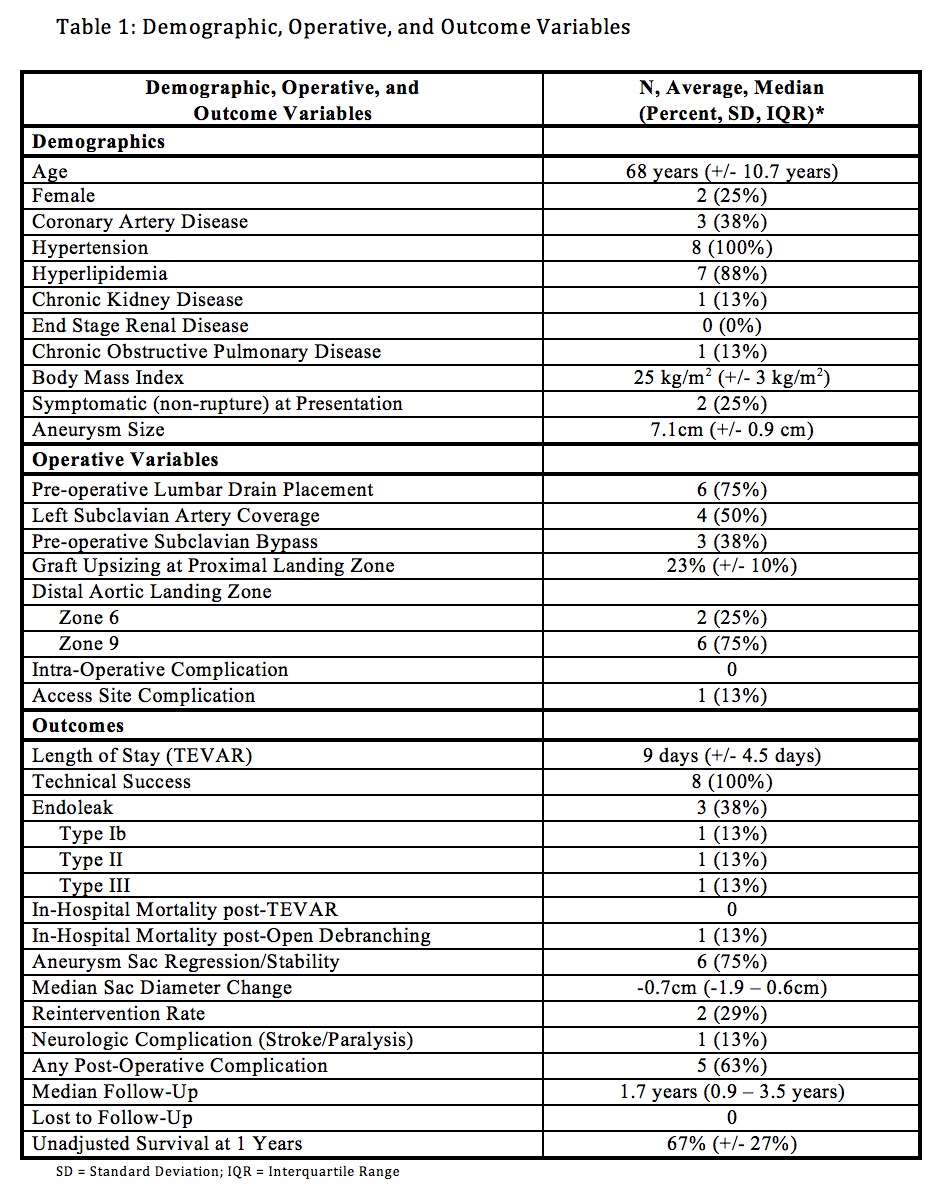
Back to 2020 ePosters
