Evolution Of Surgical Treatment Of Aortic Aneurysm: Two Decades Of Experience
Erin Greenleaf, MD, Luis Sanchez, MD, Jeffrey Jim, MD.
Washington University in St. Louis, St. Louis, MO, USA.
OBJECTIVES: The introduction of endovascular (ENDO) abdominal aortic aneurysm repair (EVAR), thoracic aneurysm repair (TEVAR) and fenestrated endografts (FEVAR) have revolutionized the treatment of aortic aneurysm disease over the past two decades. The purpose of this study is to assess the evolution of the surgical treatment of aortic aneurysmal disease over the past two decades.
METHODS: A retrospective review was performed on billing records from 1999 to 2018 at a single academic referral center. Procedures were identified using CPT (Current Procedural Terminology) codes specific for treatment of aortic aneurysmal disease. For the analysis, the 20 years was further subdivided into three time periods: “post-EVAR” (1999-2005); “post-TEVAR” (2006-2011); and “post-FEVAR” (2012-2018).
RESULTS: During the 20 year study period, there were a total of 3,994 cases (200 cases/year) identified with 1309 (33%) OAR and 2685 (67%) ENDO procedures. The number of procedures performed during the three time periods is as shown in Table 1. While there has been an increase in total number of aortic procedures during the three study periods, there has been a decline in the number of OARs. The overall number of infrarenal interventions has also declined with a concomitant increase in TEVAR and FEVAR. In the post-FEVAR period, 23% of all ENDO abdominal aortic aneurysm repairs are done with FEVAR.
CONCLUSIONS: Over the past two decades, our center has shown a rapid adoption of newer endovascular techniques to treat aortic aneurysmal disease. Despite this, our center continues to provide trainees with a robust experience in OAR. The decline in infrarenal procedures coupled with an increasing advanced aortic interventions reflects a pattern of referral to a high volume aortic center for complex patients. The implications of these findings on future vascular surgical training and certification will need to be further investigated. 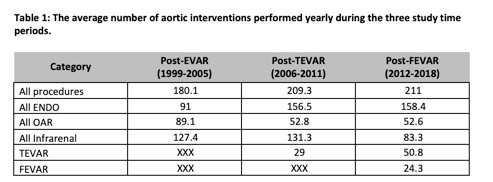
Back to 2020 ePosters
